How To Treat Acid Reflux Back Pain Immediately
Acid reflux back pain can be a debilitating and frustrating condition, affecting millions of people worldwide. If you're one of them, you're likely searching for ways to alleviate the discomfort and get back to your normal life. Fortunately, there are effective ways to treat acid reflux back pain immediately. To start, it's essential to understand the underlying causes of acid reflux back pain, which we'll explore in the next section, "Understanding Acid Reflux Back Pain." Once you grasp the root of the issue, you can move on to finding immediate relief, which we'll discuss in "Immediate Relief for Acid Reflux Back Pain." Finally, to prevent future episodes, we'll delve into long-term solutions in "Long-Term Solutions for Acid Reflux Back Pain." By the end of this article, you'll be equipped with the knowledge and strategies to tackle acid reflux back pain and regain control over your life.
Understanding Acid Reflux Back Pain
Acid reflux back pain is a common symptom experienced by many individuals who suffer from acid reflux disease. It is essential to understand the relationship between acid reflux and back pain to effectively manage and alleviate the discomfort. In this article, we will delve into the world of acid reflux back pain, exploring what it is, its causes, and its symptoms. By understanding these aspects, individuals can better navigate their condition and seek appropriate treatment. So, let's start by examining what acid reflux back pain is and how it affects the body.
What is Acid Reflux Back Pain?
Acid reflux back pain is a common symptom experienced by individuals who suffer from gastroesophageal reflux disease (GERD). It occurs when stomach acid flows back up into the esophagus, causing irritation and inflammation in the chest and back area. The pain can range from mild to severe and is often described as a burning or aching sensation in the upper and middle back, between the shoulder blades, or in the lower back. In some cases, the pain can radiate to the arms, neck, or jaw, making it difficult to distinguish from other types of back pain. Acid reflux back pain can be triggered by various factors, including eating certain foods, lying down after meals, or wearing tight clothing that puts pressure on the stomach. It can also be a sign of an underlying condition, such as a hiatal hernia or a weakened lower esophageal sphincter. If left untreated, acid reflux back pain can lead to complications, such as esophagitis, stricture, or Barrett's esophagus. Therefore, it is essential to seek medical attention if the pain persists or worsens over time. A healthcare professional can diagnose acid reflux back pain through a physical examination, medical history, and diagnostic tests, such as endoscopy or ambulatory acid probe tests. Treatment options may include lifestyle changes, over-the-counter medications, or prescription medications to reduce acid production and alleviate symptoms. In severe cases, surgery may be necessary to repair the lower esophageal sphincter or remove damaged tissue. By understanding the causes and symptoms of acid reflux back pain, individuals can take steps to manage their condition and prevent complications.
Causes of Acid Reflux Back Pain
Acid reflux back pain is a common symptom experienced by many individuals who suffer from gastroesophageal reflux disease (GERD). The causes of acid reflux back pain can be attributed to several factors. One of the primary causes is the regurgitation of stomach acid into the esophagus, which can irritate the nerves and muscles in the back, leading to pain and discomfort. Another cause is the relaxation of the lower esophageal sphincter (LES), which allows stomach acid to flow back up into the esophagus and cause irritation. Additionally, a hiatal hernia, where the stomach bulges up into the chest through an opening in the diaphragm, can also contribute to acid reflux back pain. Furthermore, certain foods and drinks, such as citrus fruits, tomatoes, chocolate, and caffeine, can trigger acid reflux and back pain in some individuals. Other factors, such as obesity, pregnancy, and smoking, can also increase the risk of developing acid reflux back pain. It is essential to identify the underlying causes of acid reflux back pain to develop an effective treatment plan and alleviate symptoms.
Symptoms of Acid Reflux Back Pain
Acid reflux back pain can manifest in various ways, and it's essential to recognize the symptoms to seek timely medical attention. The most common symptoms include a burning sensation in the chest and upper back, which can radiate to the arms, neck, and jaw. This discomfort can worsen after eating, lying down, or bending over. Some people may experience a sour or bitter taste in the mouth, regurgitation of food, and difficulty swallowing. Additionally, acid reflux back pain can cause bloating, gas, and abdominal discomfort, which can be mistaken for other conditions. In severe cases, acid reflux can lead to chronic coughing, wheezing, and shortness of breath. It's crucial to note that some individuals may not experience heartburn at all, and their primary symptom may be back pain, which can be a dull ache or a sharp, stabbing sensation. If you're experiencing any of these symptoms, it's essential to consult with your doctor to determine the best course of treatment and prevent long-term complications.
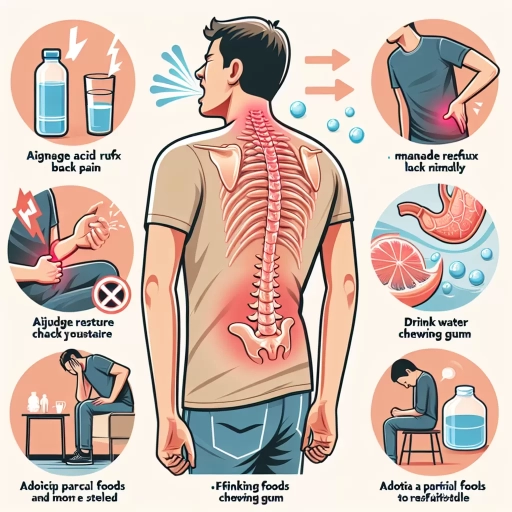
Immediate Relief for Acid Reflux Back Pain
Acid reflux back pain can be a debilitating and frustrating condition, affecting millions of people worldwide. The burning sensation and discomfort can be overwhelming, making it challenging to perform daily activities. Fortunately, there are various ways to find immediate relief from acid reflux back pain. For those seeking quick solutions, over-the-counter medications can provide fast relief. Additionally, natural remedies such as ginger, aloe vera, and licorice root have been shown to alleviate symptoms. Furthermore, simple home remedies like elevating the head of the bed, avoiding trigger foods, and practicing relaxation techniques can also bring instant relief. In this article, we will explore these options in more detail, starting with over-the-counter medications that can provide quick relief from acid reflux back pain.
Over-the-Counter Medications for Quick Relief
Over-the-counter (OTC) medications can provide quick relief for acid reflux back pain. Antacids, such as Tums, Rolaids, and Mylanta, work by neutralizing stomach acid and can provide fast relief from heartburn and back pain. Histamine-2 (H2) blockers, like ranitidine (Zantac) and famotidine (Pepcid), reduce acid production in the stomach and can also help alleviate back pain. Proton pump inhibitors (PPIs), such as omeprazole (Prilosec) and lansoprazole (Prevacid), block the production of stomach acid and can provide longer-lasting relief from acid reflux back pain. Additionally, acid reducers like aluminum hydroxide (Amphojel) and magnesium hydroxide (Milk of Magnesia) can help neutralize stomach acid and provide quick relief. It's essential to follow the recommended dosage and consult with a healthcare professional before taking any OTC medication, especially if you have a history of underlying medical conditions or take prescription medications. By taking the right OTC medication, you can quickly alleviate acid reflux back pain and get back to your daily activities.
Natural Remedies for Instant Relief
Here is the paragraphy: For instant relief from acid reflux back pain, consider incorporating natural remedies into your treatment plan. Ginger has potent anti-inflammatory properties that can help reduce inflammation and alleviate pain. You can try ginger tea, ginger ale, or add fresh ginger to your meals. Aloe vera juice is another natural remedy that can help soothe the esophagus and reduce inflammation. Slippery elm, a natural demulcent, can help protect the mucous membranes in the esophagus and reduce inflammation. Licorice root, which has anti-inflammatory properties, can also help soothe the stomach and reduce acid production. Additionally, drinking plenty of water and avoiding trigger foods can help alleviate symptoms. You can also try over-the-counter antacids or acid reducers, such as Tums, Rolaids, or Zantac, to help neutralize stomach acid and provide quick relief. Furthermore, practicing stress-reducing techniques like deep breathing, meditation, or yoga can help manage stress, which can exacerbate acid reflux symptoms. By incorporating these natural remedies and lifestyle changes, you can find instant relief from acid reflux back pain and improve your overall digestive health.
Home Remedies for Fast Relief
Here is the paragraphy: For fast relief from acid reflux back pain, try these home remedies. Ginger has natural anti-inflammatory properties that can help reduce inflammation and alleviate pain. You can make ginger tea by steeping fresh ginger in hot water or take ginger in capsule form. Aloe vera juice is another natural remedy that can help soothe the esophagus and reduce inflammation. Drinking aloe vera juice after meals can help reduce symptoms of acid reflux. Baking soda can also help neutralize stomach acid and provide quick relief from heartburn and back pain. Mix one teaspoon of baking soda with water to create a natural antacid. Additionally, practicing good posture, avoiding tight clothing, and taking regular breaks to stretch can help reduce pressure on the stomach and alleviate back pain. Elevating the head of your bed by six inches can also help prevent stomach acid from flowing up into the esophagus while you sleep. By incorporating these home remedies into your daily routine, you can find fast relief from acid reflux back pain and improve your overall quality of life.
Long-Term Solutions for Acid Reflux Back Pain
Acid reflux back pain is a common symptom experienced by many individuals who suffer from gastroesophageal reflux disease (GERD). While it can be uncomfortable and disrupt daily life, there are several long-term solutions that can help alleviate this issue. To effectively manage acid reflux back pain, it is essential to adopt a multi-faceted approach that incorporates dietary changes, lifestyle modifications, and medical treatments. By making informed choices about the food we eat, we can significantly reduce the occurrence of acid reflux back pain. Dietary changes, such as avoiding trigger foods and incorporating alkaline-rich foods, can help prevent acid reflux back pain. By understanding the impact of diet on acid reflux, individuals can take the first step towards a pain-free life. In the following section, we will explore the specific dietary changes that can help prevent acid reflux back pain.
Dietary Changes to Prevent Acid Reflux Back Pain
Dietary changes can play a significant role in preventing acid reflux back pain. One of the most effective ways to alleviate symptoms is to adopt a low-acid diet, which involves avoiding trigger foods that can irritate the stomach and cause acid reflux. Foods that are high in fat, citrus fruits, tomatoes, chocolate, spicy foods, and caffeine are common culprits that can exacerbate acid reflux. Instead, focus on incorporating alkaline-rich foods such as lean proteins, whole grains, and vegetables into your diet. Additionally, eating smaller, more frequent meals throughout the day can help reduce symptoms by putting less pressure on the lower esophageal sphincter. Drinking plenty of water and limiting carbonated beverages can also help to dilute stomach acid and reduce discomfort. Furthermore, incorporating ginger, aloe vera, and licorice root into your diet may help to soothe the stomach and reduce inflammation. By making these dietary changes, individuals can help to prevent acid reflux back pain and alleviate symptoms, promoting a healthier and more comfortable digestive system.
Lifestyle Modifications to Reduce Acid Reflux Back Pain
Lifestyle modifications play a crucial role in reducing acid reflux back pain. One of the most effective ways to alleviate symptoms is to maintain a healthy weight, as excess weight can put pressure on the stomach, causing acid to flow back up into the esophagus. Eating smaller, more frequent meals can also help reduce symptoms, as it puts less pressure on the lower esophageal sphincter. Additionally, avoiding trigger foods such as citrus fruits, tomatoes, chocolate, and spicy or fatty foods can help reduce acid production. Raising the head of the bed by 6-8 inches can also help prevent stomach acid from flowing back up into the esophagus while sleeping. Furthermore, quitting smoking and reducing stress through relaxation techniques such as deep breathing, yoga, or meditation can also help alleviate symptoms. Drinking plenty of water and limiting caffeine and alcohol consumption can also help reduce acid reflux back pain. By incorporating these lifestyle modifications into daily routine, individuals can significantly reduce their acid reflux back pain and improve their overall quality of life.
Medical Treatments for Chronic Acid Reflux Back Pain
Medical treatments for chronic acid reflux back pain often involve a combination of lifestyle modifications, medications, and in some cases, surgery. Over-the-counter antacids and acid reducers, such as Tums, Rolaids, and Zantac, can provide quick relief from acid reflux symptoms. However, for chronic cases, prescription medications like proton pump inhibitors (PPIs) and histamine-2 (H2) blockers may be necessary to reduce stomach acid production. PPIs, such as omeprazole and lansoprazole, work by blocking the production of stomach acid, while H2 blockers, like ranitidine and famotidine, reduce acid production by blocking histamine receptors. In severe cases, surgery may be required to strengthen the lower esophageal sphincter (LES) and prevent acid reflux. Laparoscopic fundoplication, a minimally invasive surgical procedure, is often used to treat chronic acid reflux. Additionally, medications like baclofen and metoclopramide can help strengthen the LES and improve gastric emptying, reducing symptoms of acid reflux back pain. It's essential to consult a healthcare professional to determine the best course of treatment for chronic acid reflux back pain, as they can help develop a personalized treatment plan that addresses the underlying causes of the condition.