How To Stay In Sinus Rhythm After Cardioversion
Cardioversion is a medical procedure that aims to restore a normal heart rhythm, also known as sinus rhythm, in individuals with abnormal heart rhythms, such as atrial fibrillation. While cardioversion can be an effective treatment, maintaining sinus rhythm after the procedure can be a challenge. To increase the chances of staying in sinus rhythm, it is essential to take a comprehensive approach that involves preparation before the procedure, lifestyle changes, and ongoing monitoring and maintenance after cardioversion. In this article, we will explore the key strategies for maintaining sinus rhythm after cardioversion, starting with the crucial step of pre-cardioversion preparation. By understanding the importance of pre-cardioversion preparation, individuals can set themselves up for success and increase their chances of staying in sinus rhythm.
Pre-Cardioversion Preparation
Pre-cardioversion preparation is a crucial step in ensuring the success of the procedure. To increase the chances of a successful cardioversion, it is essential to optimize medications, address underlying conditions, and carefully plan the timing and scheduling of the procedure. Optimizing medications involves adjusting the patient's current medication regimen to minimize the risk of complications and ensure the best possible outcome. This may include discontinuing certain medications, such as anticoagulants, and starting others, such as anti-arrhythmics. By carefully managing medications, healthcare providers can reduce the risk of bleeding, stroke, and other complications. In the next section, we will take a closer look at the importance of optimizing medications in pre-cardioversion preparation.
Optimizing Medications
Optimizing medications is a crucial step in pre-cardioversion preparation. The goal is to ensure that the medications are working effectively to control heart rhythm and reduce the risk of complications. The first step is to review the patient's current medication regimen and adjust as needed. This may involve discontinuing certain medications that can interfere with cardioversion, such as anti-arrhythmic medications, and starting or increasing others that can help maintain sinus rhythm, such as beta blockers or anti-coagulants. It's also essential to ensure that the patient is taking the correct dose of their medications and that they are not experiencing any adverse effects. Additionally, the patient's electrolyte levels, particularly potassium and magnesium, should be checked and corrected if necessary, as imbalances can increase the risk of complications during cardioversion. By optimizing medications, healthcare providers can help reduce the risk of complications and improve the chances of successful cardioversion.
Addressing Underlying Conditions
Cardioversion is a medical procedure that aims to restore a normal heart rhythm in individuals with arrhythmias, such as atrial fibrillation. However, for the procedure to be successful and the normal rhythm to be sustained, it is crucial to address any underlying conditions that may be contributing to the arrhythmia. This includes managing conditions such as high blood pressure, heart failure, and coronary artery disease, as these can increase the risk of arrhythmia recurrence. Additionally, identifying and treating underlying conditions such as sleep apnea, thyroid disorders, and electrolyte imbalances can also help to reduce the risk of arrhythmia recurrence. Furthermore, addressing lifestyle factors such as obesity, smoking, and excessive alcohol consumption can also play a crucial role in maintaining a normal heart rhythm. By addressing these underlying conditions and lifestyle factors, individuals can increase the chances of a successful cardioversion and reduce the risk of arrhythmia recurrence, ultimately improving their overall quality of life.
Cardioversion Timing and Scheduling
Cardioversion timing and scheduling are crucial factors to consider when preparing for the procedure. The timing of cardioversion is typically determined by the patient's underlying heart condition, the presence of any symptoms, and the overall health status. In general, cardioversion is usually scheduled as an outpatient procedure, and the timing is often dependent on the availability of the electrophysiology lab and the physician's schedule. Ideally, cardioversion should be performed when the patient is in a stable condition, and any underlying medical conditions are well-controlled. The procedure is usually scheduled in the morning, and the patient is advised to arrive at the hospital or clinic at least 2 hours prior to the scheduled time. This allows for adequate preparation, including the administration of any necessary medications, and the placement of electrodes and other monitoring devices. In some cases, cardioversion may be performed on an urgent basis, such as in patients with severe symptoms or those who are at risk of developing complications. In these situations, the procedure may be scheduled at short notice, and the patient may be required to arrive at the hospital or clinic immediately. Overall, the timing and scheduling of cardioversion are critical components of the procedure, and careful planning is essential to ensure a successful outcome.
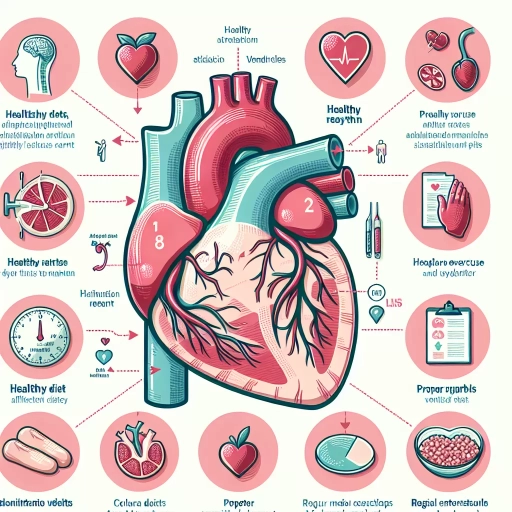
Lifestyle Changes for Sinus Rhythm Maintenance
Maintaining a healthy sinus rhythm is crucial for overall cardiovascular well-being. To achieve this, it is essential to adopt a holistic approach that incorporates various lifestyle changes. A well-balanced diet, stress management, and regular physical activity are key components of a heart-healthy lifestyle. By making informed dietary choices, individuals can significantly reduce their risk of developing conditions that can disrupt sinus rhythm. A diet rich in fruits, vegetables, whole grains, and lean proteins can help maintain healthy blood pressure, cholesterol levels, and blood sugar levels. Furthermore, stress reduction techniques such as meditation, yoga, and deep breathing exercises can help mitigate the negative impact of stress on the heart. Regular exercise and physical activity can also help improve cardiovascular health by strengthening the heart and increasing blood flow. By incorporating these lifestyle changes, individuals can significantly improve their chances of maintaining a healthy sinus rhythm. By starting with dietary modifications, individuals can set themselves up for success and create a strong foundation for overall heart health.
Dietary Modifications for Heart Health
A well-planned diet plays a crucial role in maintaining heart health, particularly for individuals who have undergone cardioversion to restore a normal sinus rhythm. Dietary modifications can help reduce the risk of arrhythmias, lower blood pressure, and prevent cardiovascular disease. A heart-healthy diet should focus on increasing the intake of omega-3 fatty acids, antioxidants, and fiber-rich foods. Fatty fish like salmon, mackerel, and sardines are rich in omega-3 fatty acids, which help reduce inflammation and improve heart function. Antioxidant-rich foods like berries, leafy greens, and other fruits and vegetables can help protect against oxidative stress and inflammation. Whole grains, legumes, and nuts are rich in fiber, which can help lower cholesterol levels and regulate blood sugar. Additionally, limiting the intake of processed and packaged foods, sugary drinks, and saturated fats is essential. The Mediterranean diet, which emphasizes whole grains, fruits, vegetables, and healthy fats, has been shown to be effective in reducing the risk of cardiovascular disease and promoting heart health. By incorporating these dietary modifications into their lifestyle, individuals can reduce their risk of arrhythmias and maintain a healthy sinus rhythm.
Stress Reduction Techniques
Stress reduction techniques are essential for maintaining a healthy lifestyle, particularly for individuals who have undergone cardioversion to restore a normal sinus rhythm. Chronic stress can lead to an increase in stress hormones like cortisol and adrenaline, which can disrupt the body's natural rhythm and increase the risk of arrhythmias. Fortunately, there are several effective stress reduction techniques that can help mitigate this risk. One of the most popular techniques is meditation, which involves focusing the mind on a specific object, thought, or activity to achieve a mentally clear and emotionally calm state. Regular meditation practice has been shown to reduce stress and anxiety, lower blood pressure, and improve overall cardiovascular health. Another technique is deep breathing exercises, which involve slow, deliberate breaths to calm the nervous system and reduce stress hormones. Yoga is also an excellent stress reduction technique, combining physical postures, breathing techniques, and meditation to promote relaxation and reduce stress. Additionally, engaging in regular physical activity, such as walking or jogging, can help reduce stress and anxiety by releasing endorphins, also known as "feel-good" hormones. Other stress reduction techniques include progressive muscle relaxation, visualization, and mindfulness-based stress reduction. By incorporating these techniques into daily life, individuals can effectively manage stress and reduce the risk of arrhythmias, promoting a healthy sinus rhythm and overall well-being.
Regular Exercise and Physical Activity
Regular exercise and physical activity are essential for maintaining overall health and well-being, and they also play a crucial role in supporting sinus rhythm maintenance. Engaging in regular physical activity can help to reduce stress and anxiety, which are common triggers for arrhythmias. Exercise can also improve cardiovascular health by strengthening the heart and increasing blood flow, which can help to reduce the risk of arrhythmias. Additionally, regular physical activity can help to improve sleep quality, which is also important for maintaining a healthy heart rhythm. The American Heart Association recommends at least 150 minutes of moderate-intensity aerobic physical activity or 75 minutes of vigorous-intensity aerobic physical activity per week, or a combination of both. It's also important to incorporate strength-training exercises into your routine, as this can help to improve overall muscle function and reduce the risk of injury. Some examples of moderate-intensity aerobic exercises include brisk walking, cycling, and swimming, while vigorous-intensity aerobic exercises include running, jumping rope, and boxing. It's always a good idea to consult with your doctor before starting a new exercise program, especially if you have any underlying health conditions or concerns. By incorporating regular exercise and physical activity into your lifestyle, you can help to support sinus rhythm maintenance and reduce your risk of arrhythmias.
Post-Cardioversion Monitoring and Maintenance
After a successful cardioversion procedure, it is essential to undergo post-cardioversion monitoring and maintenance to ensure the heart returns to a normal rhythm and remains that way. This period is crucial in preventing complications and reducing the risk of atrial fibrillation recurrence. A comprehensive post-cardioversion care plan typically involves regular follow-up appointments and check-ups with a healthcare provider to monitor the heart's rhythm and adjust treatment plans as needed. Additionally, patients may need to undergo continuous monitoring for atrial fibrillation recurrence, which can be done using various devices and techniques. Furthermore, medications and treatment plans may need to be adjusted to prevent future episodes of atrial fibrillation. By closely monitoring the heart's rhythm and making necessary adjustments, patients can reduce their risk of complications and improve their overall quality of life. Regular follow-up appointments and check-ups are a critical component of post-cardioversion care, and patients should be prepared to work closely with their healthcare provider to ensure a smooth and successful recovery.
Follow-up Appointments and Check-ups
Follow-up appointments and check-ups are crucial after cardioversion to ensure that the heart is maintaining a normal sinus rhythm and to monitor for any potential complications. Regular check-ups with a cardiologist or healthcare provider will help to assess the effectiveness of the cardioversion procedure and identify any signs of arrhythmia recurrence. During these appointments, the healthcare provider will typically perform an electrocardiogram (ECG) to check the heart's rhythm and may also conduct a physical examination to look for any signs of heart failure or other complications. Additionally, the healthcare provider may adjust medications or recommend lifestyle changes to help maintain a normal heart rhythm. It is essential to keep all scheduled follow-up appointments and to report any symptoms or concerns to the healthcare provider promptly. By doing so, individuals can help ensure that their heart remains in a normal sinus rhythm and reduce the risk of complications. Furthermore, regular check-ups can also help to identify any underlying conditions that may be contributing to arrhythmia, such as high blood pressure or sleep apnea, and allow for early intervention and treatment. Overall, follow-up appointments and check-ups are a critical component of post-cardioversion care and play a vital role in maintaining a healthy heart rhythm.
Monitoring for Atrial Fibrillation Recurrence
Monitoring for atrial fibrillation recurrence is a crucial aspect of post-cardioversion care. After a successful cardioversion, patients are at risk of experiencing atrial fibrillation recurrence, which can occur within days, weeks, or even months after the procedure. To minimize this risk, regular monitoring is essential to detect any signs of atrial fibrillation recurrence. This can be achieved through various methods, including electrocardiogram (ECG) monitoring, Holter monitoring, and mobile cardiac telemetry. ECG monitoring involves recording the heart's electrical activity at regular intervals, while Holter monitoring involves wearing a portable device that records the heart's activity over a 24-hour period. Mobile cardiac telemetry, on the other hand, involves wearing a small device that continuously monitors the heart's activity and transmits data to a monitoring center. By regularly monitoring for atrial fibrillation recurrence, healthcare providers can quickly identify any abnormalities and take prompt action to prevent further complications. Additionally, patients can also play an active role in monitoring their condition by tracking their symptoms and reporting any changes to their healthcare provider. By working together, patients and healthcare providers can reduce the risk of atrial fibrillation recurrence and maintain a healthy sinus rhythm.
Adjusting Medications and Treatment Plans
Adjusting medications and treatment plans is a crucial step in maintaining sinus rhythm after cardioversion. The goal is to prevent the return of atrial fibrillation and minimize the risk of complications. Medications such as anti-arrhythmics, beta blockers, and anticoagulants may need to be adjusted or changed to optimize their effectiveness. For example, if a patient is taking an anti-arrhythmic medication, the dosage may need to be increased or decreased to achieve the desired effect. Similarly, beta blockers may need to be adjusted to control heart rate and blood pressure. Anticoagulants, such as warfarin, may need to be continued or discontinued based on the patient's individual risk factors for stroke and bleeding. In addition to medication adjustments, treatment plans may also need to be modified to address underlying conditions that may be contributing to atrial fibrillation, such as hypertension, sleep apnea, or thyroid disorders. Lifestyle changes, such as increasing physical activity, losing weight, and reducing stress, may also be recommended to help maintain sinus rhythm. Regular follow-up appointments with a healthcare provider are essential to monitor the effectiveness of treatment plans and make any necessary adjustments. By working closely with a healthcare provider, patients can optimize their treatment plan and reduce the risk of atrial fibrillation recurrence.