How Long Can You Live With Pleural Effusion
Pleural effusion is a condition where fluid accumulates in the pleural space, which is the area between the lungs and the chest wall. This condition can be caused by various factors, including infections, cancer, and heart failure. The prognosis for individuals with pleural effusion varies depending on the underlying cause and the severity of the condition. In this article, we will explore the life expectancy of individuals with pleural effusion, as well as the management and treatment options available. To understand the life expectancy and treatment options, it is essential to first understand what pleural effusion is and how it affects the body. We will delve into the details of pleural effusion, including its causes, symptoms, and diagnosis. Additionally, we will discuss the life expectancy of individuals with pleural effusion and the factors that influence it. Finally, we will examine the management and treatment options available for pleural effusion, including medications, procedures, and lifestyle changes. By understanding these aspects, individuals with pleural effusion can better manage their condition and improve their quality of life. Understanding the basics of pleural effusion is crucial, so let's start by exploring what it is and how it affects the body.
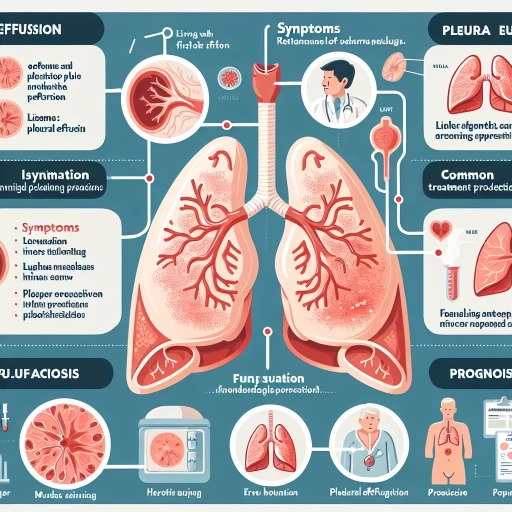
Understanding Pleural Effusion
Pleural effusion is a condition characterized by the accumulation of fluid in the pleural space, which is the area between the lungs and the chest wall. This condition can be caused by a variety of factors, including infections, injuries, and certain medical conditions. Understanding the causes and risk factors of pleural effusion is crucial in determining the best course of treatment. There are also different types of pleural effusion, each with its own unique characteristics and treatment options. In this article, we will delve into the world of pleural effusion, starting with the basics of what it is, followed by an exploration of its causes and risk factors, and finally, a discussion of the different types of pleural effusion. By the end of this article, readers will have a comprehensive understanding of pleural effusion and its various aspects. So, let's begin by understanding what pleural effusion is.
What is Pleural Effusion?
Pleural effusion is a medical condition characterized by the accumulation of excess fluid in the pleural space, which is the thin gap between the lungs and the chest wall. This fluid buildup can be caused by a variety of factors, including infections, injuries, cancer, and certain medical conditions such as heart failure, kidney disease, and liver disease. The excess fluid can put pressure on the lungs, making it difficult to breathe and leading to symptoms such as shortness of breath, chest pain, and coughing. In some cases, pleural effusion can be a life-threatening condition if left untreated, as it can lead to respiratory failure and other complications. Treatment options for pleural effusion depend on the underlying cause and may include drainage of the fluid, antibiotics, and other medications to manage symptoms and address the underlying condition. In severe cases, hospitalization may be necessary to provide supportive care and monitor the patient's condition closely. Understanding the causes, symptoms, and treatment options for pleural effusion is essential for effective management of the condition and improving patient outcomes.
Causes and Risk Factors of Pleural Effusion
Pleural effusion is a complex condition that can arise from a multitude of causes and risk factors. The primary cause of pleural effusion is an imbalance in the production and absorption of fluid in the pleural space, which can be triggered by various underlying conditions. One of the most common causes of pleural effusion is congestive heart failure, which can lead to fluid buildup in the pleural space due to increased pressure in the pulmonary veins. Other cardiovascular conditions, such as coronary artery disease, cardiomyopathy, and pulmonary embolism, can also contribute to the development of pleural effusion. Additionally, lung diseases like pneumonia, tuberculosis, and lung cancer can cause inflammation and scarring in the pleural tissue, leading to fluid accumulation. Furthermore, kidney disease, liver disease, and autoimmune disorders like lupus and rheumatoid arthritis can also increase the risk of developing pleural effusion. Other risk factors include chest trauma, surgery, and certain medications like diuretics and beta-blockers. In some cases, pleural effusion can also be caused by infections like empyema, which is a bacterial infection of the pleural space. It is essential to identify the underlying cause of pleural effusion to develop an effective treatment plan and manage the condition effectively.
Types of Pleural Effusion
Pleural effusion is a condition characterized by the accumulation of fluid in the pleural space, which is the area between the lungs and the chest wall. There are several types of pleural effusion, each with distinct causes and characteristics. Transudative pleural effusion is the most common type, accounting for approximately 50% of cases. It occurs when fluid leaks from the blood vessels into the pleural space due to increased pressure or decreased oncotic pressure. This type of effusion is often seen in conditions such as congestive heart failure, liver cirrhosis, and nephrotic syndrome. Exudative pleural effusion, on the other hand, is caused by inflammation or infection, leading to the accumulation of fluid rich in protein and cells. This type of effusion is commonly associated with conditions such as pneumonia, tuberculosis, and lung cancer. Hemorrhagic pleural effusion is a rare type of effusion characterized by the presence of blood in the pleural fluid, often due to trauma or malignancy. Chylous pleural effusion is another rare type, caused by the leakage of lymphatic fluid into the pleural space, often due to trauma or malignancy. Lastly, empyemic pleural effusion is a type of effusion characterized by the presence of pus in the pleural fluid, often due to bacterial infection. Understanding the different types of pleural effusion is crucial for accurate diagnosis and treatment.
Life Expectancy with Pleural Effusion
Pleural effusion is a condition characterized by the accumulation of fluid in the pleural space of the lungs, which can significantly impact an individual's quality of life and life expectancy. The prognosis for individuals with pleural effusion varies widely depending on several factors, including the underlying cause of the condition, the severity of symptoms, and the effectiveness of treatment. Understanding the factors that affect life expectancy with pleural effusion is crucial for developing an effective treatment plan and improving patient outcomes. In this article, we will explore the factors that affect life expectancy with pleural effusion, examine the survival rates for different types of pleural effusion, and discuss the impact of treatment on life expectancy. By understanding these key aspects, individuals with pleural effusion can better navigate their condition and make informed decisions about their care. Factors affecting life expectancy with pleural effusion are numerous and complex, and will be discussed in the following section.
Factors Affecting Life Expectancy with Pleural Effusion
Pleural effusion is a condition characterized by the accumulation of fluid in the pleural space, which can significantly impact life expectancy. Several factors can influence life expectancy in individuals with pleural effusion, including the underlying cause of the condition, the severity of the effusion, and the effectiveness of treatment. The underlying cause of pleural effusion, such as cancer, heart failure, or pneumonia, plays a crucial role in determining life expectancy. For instance, individuals with malignant pleural effusion, which is often associated with lung cancer, have a poorer prognosis compared to those with non-malignant causes. The severity of the effusion, measured by the amount of fluid accumulated and the degree of lung compression, also affects life expectancy. Large effusions can lead to respiratory failure, which can be life-threatening if left untreated. Additionally, the presence of other comorbidities, such as chronic obstructive pulmonary disease (COPD) or kidney disease, can further reduce life expectancy. Treatment options, including thoracentesis, pleurodesis, and chemotherapy, can also impact life expectancy. In some cases, treatment can improve symptoms and prolong life, while in others, it may only provide palliative care. Overall, life expectancy with pleural effusion varies widely depending on individual factors, and a comprehensive evaluation by a healthcare professional is necessary to determine the best course of treatment and estimate life expectancy.
Survival Rates for Different Types of Pleural Effusion
The survival rate for different types of pleural effusion varies significantly depending on the underlying cause, patient's overall health, and treatment response. Malignant pleural effusion, which is associated with cancer, has a generally poor prognosis, with a median survival time of 3-12 months. In contrast, patients with benign pleural effusion, such as those caused by pneumonia or heart failure, have a significantly better prognosis, with a median survival time of 1-2 years or more. Tuberculous pleural effusion, which is caused by tuberculosis, has a variable prognosis, with a median survival time of 6-24 months, depending on the effectiveness of treatment. Parapneumonic pleural effusion, which is associated with pneumonia, has a relatively good prognosis, with a median survival time of 1-2 years. However, the survival rate can be significantly improved with prompt and effective treatment, including antibiotics and drainage of the effusion. It's essential to note that these survival rates are general estimates and can vary significantly depending on individual factors, such as the patient's age, overall health, and response to treatment.
Impact of Treatment on Life Expectancy
The impact of treatment on life expectancy for individuals with pleural effusion varies significantly depending on the underlying cause, the effectiveness of the treatment, and the overall health of the patient. Generally, treatment can improve life expectancy by managing symptoms, reducing the accumulation of fluid, and addressing the underlying condition. For example, if the pleural effusion is caused by a treatable condition such as pneumonia or heart failure, effective treatment of the underlying condition can lead to a significant improvement in life expectancy. In some cases, treatment can even lead to a complete resolution of the pleural effusion, resulting in a normal life expectancy. However, if the pleural effusion is caused by a more serious condition such as cancer, the impact of treatment on life expectancy is often more limited. In these cases, treatment may focus on managing symptoms and improving quality of life, rather than curing the underlying condition. Despite this, treatment can still play an important role in improving life expectancy, even if it is not curative. For instance, chemotherapy and radiation therapy can help to slow the progression of cancer, leading to an improvement in life expectancy. Additionally, palliative care, which focuses on managing symptoms and improving quality of life, can also play an important role in improving life expectancy. Overall, the impact of treatment on life expectancy for individuals with pleural effusion is highly variable and depends on a range of factors, including the underlying cause, the effectiveness of treatment, and the overall health of the patient.
Managing and Treating Pleural Effusion
Pleural effusion is a serious medical condition characterized by the accumulation of excess fluid in the pleural space, which can cause respiratory distress, chest pain, and other complications. Managing and treating pleural effusion requires a comprehensive approach that incorporates medical treatment options, surgical interventions, and lifestyle changes. Medical treatment options, such as diuretics and antibiotics, can help alleviate symptoms and address underlying conditions. In some cases, surgical interventions, such as thoracentesis and pleurodesis, may be necessary to drain excess fluid and prevent recurrence. Additionally, lifestyle changes, such as quitting smoking and maintaining a healthy weight, can help manage symptoms and improve overall health. By understanding the various treatment options and making informed lifestyle choices, individuals with pleural effusion can effectively manage their condition and improve their quality of life. One of the most effective ways to manage pleural effusion is through medical treatment options, which will be discussed in the next section.
Medical Treatment Options for Pleural Effusion
Pleural effusion is a condition characterized by the accumulation of fluid in the pleural space, which is the area between the lungs and the chest wall. The treatment options for pleural effusion depend on the underlying cause, the severity of the condition, and the overall health of the patient. In some cases, pleural effusion may resolve on its own without treatment, but in other cases, medical intervention is necessary to manage symptoms and prevent complications. Treatment options may include thoracentesis, which is a procedure to remove excess fluid from the pleural space, or pleural drainage, which involves the insertion of a catheter to drain the fluid. In some cases, medication may be prescribed to manage symptoms such as pain, cough, and shortness of breath. In severe cases, surgery may be necessary to repair any underlying damage to the lungs or pleura. In addition, treatment may also focus on addressing the underlying cause of the pleural effusion, such as cancer, infection, or heart failure. In some cases, treatment may involve a combination of these approaches, and the patient may need to be hospitalized for close monitoring and management. Overall, the goal of treatment is to relieve symptoms, prevent complications, and improve the patient's quality of life.
Surgical Interventions for Pleural Effusion
Surgical interventions for pleural effusion are often reserved for patients who have failed conservative management or have severe symptoms. One common surgical procedure is thoracentesis, which involves the insertion of a needle or catheter into the pleural space to drain the excess fluid. This procedure can provide immediate relief from symptoms such as shortness of breath and chest pain. Another surgical option is pleurodesis, which involves the injection of a sclerosing agent into the pleural space to induce inflammation and scarring, thereby preventing the re-accumulation of fluid. In some cases, a pleural catheter may be inserted to allow for repeated drainage of the fluid. In more severe cases, surgical decortication or pleurectomy may be necessary to remove the thickened pleura and prevent further fluid accumulation. These surgical interventions can significantly improve the quality of life for patients with pleural effusion, but they also carry risks and complications, such as infection, bleeding, and respiratory failure. Therefore, surgical interventions should be carefully considered and individualized based on the patient's underlying condition, symptoms, and overall health status.
Lifestyle Changes to Manage Pleural Effusion Symptoms
Living with pleural effusion requires making significant lifestyle changes to manage symptoms and improve overall quality of life. One of the most crucial changes is to stop smoking, as it can exacerbate the condition and worsen symptoms. Additionally, maintaining a healthy weight through a balanced diet and regular exercise can help reduce pressure on the lungs and improve breathing. It's also essential to get enough rest and avoid overexertion, as fatigue can worsen symptoms. Furthermore, elevating the head of the bed by 30-40 degrees can help reduce shortness of breath and improve sleep quality. Drinking plenty of fluids, such as water and clear broths, can also help thin out mucus and make it easier to cough up. Avoiding exposure to pollutants, dust, and chemicals can also help reduce inflammation and irritation in the lungs. In some cases, oxygen therapy may be necessary to help increase oxygen levels in the blood. By making these lifestyle changes, individuals with pleural effusion can better manage their symptoms and improve their overall quality of life.