How To Tell If Pelvic Floor Is Tight Or Weak
 Understanding the often overlooked dynamics of your body can unlock the key to optimum health. One such key body area to be aware of is the Pelvic Floor, a complex structure involved in various critical functions. Recognizing the condition of your pelvic floor, be it tight or weak, predicates the onset of potential health issues. This comprehensive guide will connect you with detailed insights about the vital functionality of the pelvic floor, help you identify the distinct signs and symptoms indicating a tight or weak pelvic floor, and acquaint you with the available assessment and treatment options to address pelvic floor imbalances. As we initiate our exploration into this crucial health matter, we will delve into understanding the intrinsic functionality of the pelvic floor, setting a robust foundation for your body awareness journey.
Understanding the often overlooked dynamics of your body can unlock the key to optimum health. One such key body area to be aware of is the Pelvic Floor, a complex structure involved in various critical functions. Recognizing the condition of your pelvic floor, be it tight or weak, predicates the onset of potential health issues. This comprehensive guide will connect you with detailed insights about the vital functionality of the pelvic floor, help you identify the distinct signs and symptoms indicating a tight or weak pelvic floor, and acquaint you with the available assessment and treatment options to address pelvic floor imbalances. As we initiate our exploration into this crucial health matter, we will delve into understanding the intrinsic functionality of the pelvic floor, setting a robust foundation for your body awareness journey.Understanding the Functionality of the Pelvic Floor
In the complex structure of our body, the pelvic floor plays a crucial and often underappreciated role. To fully comprehend its significance, it's essential to delve into understanding the functionality of the pelvic floor. This involves not only looking at its basic anatomy and functions but also recognizing the importance of maintaining a balanced pelvic floor musculature. In addition, it's vital to discuss the often misunderstood topic of pelvic floor dysfunction. In the following sections, we'll start with a look at the pelvic floor's fundamental anatomy and its numerous functions that are essential for normal body functioning. Then we'll move forward to discuss the role of balanced musculature in maintaining pelvic floor health, and finally, we'll shed light on the condition known as pelvic floor dysfunction, its causes, impacts, and possible solutions. Grasping these aspects should provide a holistic understanding of the pelvic floor and its intricate functionality. Let's embark on this explorative journey beginning with the basic anatomy and functionality of the pelvic floor.
The Basic Anatomy and Functions of the Pelvic Floor
The pelvic floor is a group of muscles shaped like a hammock that stretches from the pubic bone at the front, to the coccyx (tail bone) at the back, and sidewalls to the sitting bones. It plays fundamental roles in our bodies that often go overlooked. A strong and flexible pelvic floor is pivotal for various critical functions such as supporting our internal organs- including the bowel, bladder, and in females, the uterus. The primary function of the pelvic floor is to maintain continence. These muscles provide control over the bladder and bowel by tightening to prevent leakage of urine, feces, or flatus, and relaxing to allow their release. Without a properly functioning pelvic floor, individuals may encounter issues, such as incontinence and prolapse. In women, the pelvic floor acts as a support structure for the uterus, particularly during pregnancy when the weight of the growing baby places increased pressure on these muscles. Strain on the pelvic floor muscles can lead to a predominant condition known as pelvic organ prolapse, where organs sag into the vagina, prompting discomfort and impacting overall quality of life. The pelvic floor is also key to sexual function in both men and women. Strong pelvic floor muscles enhance arousal and sensation during sexual activities. Conversely, a tight or weak pelvic floor can lead to discomfort, pain, or difficulties during intercourse. It's not all about strength, however. The ability to fully relax the pelvic floor muscles is just as important as the ability to contract them. A tense, or tight, pelvic floor may lead to pain, difficulties with intercourse, and issues with voiding urine or feces, whereas a weak pelvic floor may result in incontinence and pelvic organ prolapse. The role of your pelvic floor in maintaining your overall health cannot be overlooked. Its importance extends beyond mere physical functions to aspects that influence your mental and emotional health. Consequently, it's essential to tell if your pelvic floor is tight or weak to address it immediately.
The Importance of a Balanced Pelvic Floor Musculature
Understanding the functionality of the pelvic floor is critical, but equally crucial is appreciating the significance of balanced pelvic floor musculature. To maintaining the overall health and well-being of the body, a balanced pelvic floor musculature performs an essential role. This group of muscles at the pelvic base acts like a hammock, supporting vital organs such as the bladder, rectum, and uterus or prostate. Along with these significant responsibilities, this musculature is integral in critical functions such as sexual performance, urinary and fecal continence, and pelvic organ support. When pelvic floor muscles are either too tight or weak, a series of complications may arise. This could lead to problems such as chronic lower back pain, constipation, urinary and fecal incontinence, and sexual dysfunction. Just like any other group of muscles in the body, the pelvic floor muscles require a certain degree of flexibility and strength. By maintaining a balance, the pelvic floor can function properly, preventing possible discomfort, embarrassment, and debilitating conditions. If the pelvic floor is tight, the muscles constantly contract leading to painful or hurried urination and possibly lead to recurrent Urinary Tract Infections (UTIs) due to the inability to empty the bladder fully. On the other hand, weak pelvic floor muscles can cause difficulty in controlling the bladder and bowel. In both scenarios, sexual performance may be affected which could negatively impact mental health and relationships. Hence, understanding and maintaining a balanced pelvic floor musculature is of utmost importance. Regular exercise, healthy dietary habits, stress management techniques, and, when necessary, medical interventions can promote and preserve its balance, thereby ensuring overall wellness and quality of life. Therefore, a regular check determining whether the pelvic floor is tight or weak is significant, allowing early interventions and avoiding future complications.
Pelvic Floor Dysfunction: An Overview
Pelvic Floor Dysfunction (PFD) is a concerning health issue that often remains uncharted in general discussions. It's a complex set of conditions that occur when the muscles in the pelvic floor, a group of structures that act like a hammock to brace the pelvic organs, fail to function properly due to tightness or weakness. The primary effects are often seen in the forms of urinary or bowel inconsistencies, pain during intercourse, and profound lower back pain. The paradoxical scenario of a tight or weak pelvic floor often confounds victims,as the symptoms of both conditions bear remarkable similarities. A tight pelvic floor, also known as hypertonic dysfunction, is primarily characterized by muscle spasms and painful sex. It can occur due to various contributing factors such as stress, repetitive strain injuries, and traumatic physical events. A weak pelvic floor, or hypotonic dysfunction, is often instigated by significant physical incidents like childbirth or surgery. It frequently manifests as urinary or fecal incontinence and a feeling of pelvic heaviness. Understanding the functionality of the pelvic floor assists in discerning these conditions better. A healthy pelvic floor contracts and relaxes efficiently, allowing for seamless bowel and bladder function, providing much-needed organ support and enriching sexual performance. However, when there are disruptions in this function, it can lead to PFD. One revolutionary method of gauging whether your pelvic floor is manifesting signs of tightness or weakness is through "self-tests". These incorporate simple activities such as attempting to stop urination mid-stream or conducting a kegel exercise. While these tests are rudimentary and not definitive diagnoses, they offer a glimpse into your pelvic health and can guide you towards seeking professional medical advice if necessary. In an era where discussions about pelvic health are increasingly paving their way into general conversations, understanding the drastic effects of PFD has never been more crucial. Whether it's the discomforting tightness or the debilitating weakness of the pelvic floor, each echo an urgent call to action for affected individuals to seek immediate and comprehensive medical attention.
Signs and Symptoms of a Tight or Weak Pelvic Floor
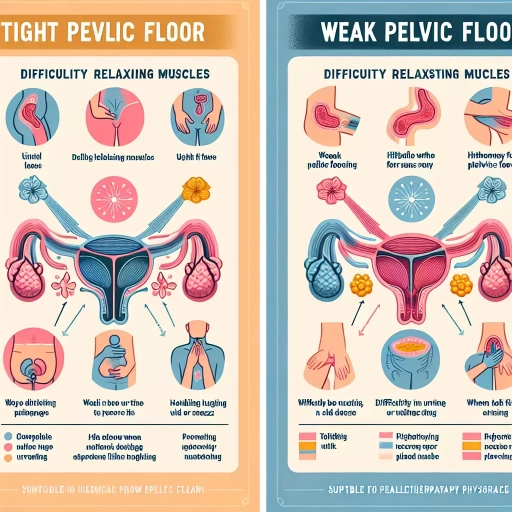
A strong, versatile pelvic floor is vital for overall health and wellbeing, but an inability to identify signs of a tight or weak pelvic floor can lead to chronic issues. This article aims to enhance your understanding of the subtle signals your body may be sending about the state of your pelvic health. We delve into the indications of a tight pelvic floor, a health issue that typically manifests in noticeable discomfort and difficulty in executing specific movements. Recognizing symptoms of a weakened pelvic floor is just as crucial, as it can contribute to incontinence and sexual dysfunction. Intriguingly, pelvic tension and laxity can coexist, presenting an unusual but significant hurdle in maintaining pelvic health. This myriad of signs and symptoms can be daunting, but understanding them is the first step towards management or recovery. As we transition into our first section, let's shed light on the indicators of a tight pelvic floor and how you can make early detection an absolute possibility.
The Indications of a Tight Pelvic Floor
Indications of a Tight Pelvic Floor Recognizing the telltale signs of a tight pelvic floor can be instrumental in diagnosing and treating pelvic floor dysfunction effectively. A tight pelvic floor can result from prolonged sitting, overworking abdominal muscles, excessive stress, or other physiological factors. One of the most common indications is chronic pelvic pain, which could manifest as a steady, ongoing discomfort or sudden, severe spasms in the area surrounding the pelvic floor. Another frequent sign is dyspareunia, or painful sexual intercourse. Women with a tight pelvic floor may experience discomfort or pain during or after sex. This pain occurs due to the heightened tension in the pelvic floor muscles, which can make sexual penetration difficult or impossible. Besides, these women might find it challenging to undergo gynecological examinations due to the discomfort caused by the vaginal speculum. Other indications of a tight pelvic floor include difficulty in voiding and bowel movements. A tight pelvic floor can create a sensation of constant fullness, leading to frequent urination or constipation. Some individuals might also experience a feeling of incomplete emptying of the bladder or bowels after using the bathroom. Moreover, lower back pain and hip pain could also serve as indicators of a tight pelvic floor. Furthermore, individuals may also encounter discomfort while sitting or wearing tight clothing. This sensation can range from slight unease to extreme discomfort depending on the severity of the pelvic floor tightness. In advanced cases, individuals may also observe signs of urinary or fecal incontinence, which can severely affect their overall quality of life. Women who are pregnant or have recently given birth are more susceptible to developing a tight pelvic floor, as the weight of the fetus or the strain of giving birth can increase tension in the pelvic muscles. Hence, these individuals need to be particularly observant of the signs and symptoms of a tight pelvic floor and report them to their healthcare provider at the earliest. The above signs and triggers highlight the importance of being aware of your bodily functions and understanding when something seems out of the ordinary. A tight pelvic floor is not something to be ignored as it can greatly impact your physical and emotional well-being. If you suspect pelvic floor tightness, seek advice from a healthcare professional who can guide you on the most effective treatment and management options to alleviate your symptoms.
Recognizing the Symptoms of a Weakened Pelvic Floor
Recognizing the Symptoms of a Weakened Pelvic Floor Recognizing the symptoms of a weakened pelvic floor is crucial in identifying and dealing with this common but often overlooked issue. The pelvic floor muscles play a pivotal role in providing support to the bladder, bowel and uterus (in women), affecting urinary and bowel functioning. A weakened pelvic floor can lead to a multitude of problems, and its symptoms are often subtle and easily misunderstood. The most common symptom is urinary incontinence, a condition characterized by involuntary loss of urine, especially experienced during physical activities that increase abdominal pressure such as lifting, sneezing or even laughing. It's common for individuals with a weakened pelvic floor to frequently feel an urgent need to urinate. Bowel incontinence or constipation could also signify a weakened pelvic floor. Struggling to sufficiently control wind is another telltale symptom. For women-specific signs, a deep ache in the lower back, or experiencing discomfort or pain during sexual intercourse may indicate issues with their pelvic floor muscles. Other less obvious symptoms can include a feeling of heaviness, pressure, or even a bulge in the pelvic area - often termed pelvic organ prolapse. This happens when the pelvic floor is unable to provide sufficient support, causing one or more of the pelvic organs to sag or drop. Pelvic organ prolapse symptoms can feel more pronounced towards the end of the day and may be relieved somewhat by lying down. It's essential to note that these symptoms can overlap with numerous separate health conditions. Hence, it's always crucial to consult with a healthcare professional for a precise diagnosis. Recognizing these symptoms early could make a significant difference in preventing further damage and managing the condition successfully. The good news is, much like any other muscle group, the pelvic floor can be strengthened through targeted exercises. Being aware of these symptoms can lead to the necessary actions, ultimately enhancing overall quality of life.
How Tightness and Weakness Can Coexist
Understanding the coexistence of tightness and weakness in the pelvic floor is crucial because it can manifest in confusing and multifaceted signs. These symptoms are often misunderstood due to the paradoxical nature of the condition. The pelvic floor, a complex network of muscles, ligaments, and tissues spanning the area beneath the pelvis, serves as a support system for our pelvic organs. A healthy pelvic floor has an ideal balance of elasticity and strength, allowing it to carry out functions like maintaining continence, supporting childbirth, and ensuring comfortable sexual intercourse. However, the peculiar phenomenon of tightness and weakness coexisting in this region can disrupt these functions, leading to a host of symptoms. Tightness in the pelvic floor, medially termed hypertonicity, entails a chronic or persisting contracture of the pelvic muscles. It's akin to the sensation of perpetually clenching your fists, causing discomfort, pain, and often leading to dyspareunia (painful intercourse). It might seem counterintuitive, but this overactivity of muscles can lead to weakness. Over time, the continuous contraction prevents the muscles from fully relaxing, eventually eroding their strength. This muscle fatigue can lead to weakness or hypotonicity, impairing the ability to control bowel movements or urination. The leakage or incontinence results from the muscles' inability to effectively contract after being incessantly tightened. Moreover, a tight pelvic floor can result in trigger points or localized spots of extreme tenderness, exacerbating the overall discomfort. It's essential to understand that the body operates synergistically; thus, an issue in one area could potentially manifest symptoms elsewhere. For example, a tight, weak pelvic floor could lead to recurrent lower back pain or hip pain. It might not immediately seem related, but once diagnosed, the relationship becomes more obvious. Navigating a tight and weak pelvic floor can be tricky due to the peculiar coexistence of signs. However, recognizing these symptoms forms a vital step in restoring balance and function in this integral part of our anatomy. Recognizing the signs and pinpointing the exact problem can be challenging, but with the right care, tailored exercises, and attention, you can recover pelvic floor muscle harmony, thereby improving your quality of life.
Assessment and Treatment Options for Pelvic Floor Imbalances
Pelvic Floor Imbalances comprise an area of health concern often overlooked, yet they hold significant bearing on quality of life. These imbalances can manifest as either a too weak or overly tight pelvic floor, leading to a myriad of inconvenient, and sometimes painful, symptoms. Thankfully, modern medicine has advanced to the point where we have professional diagnostic tools, therapeutic approaches, and effective exercises available to assess and treat these issues. This article first delves into how healthcare professionals utilize advanced diagnostic tools to discern the nature and extent of pelvic floor dysfunction. It then transitions to exploring how various therapeutic approaches aim to bring balance to a tight pelvic floor. The last section outlines exercises tailored explicitly for strengthening a weak pelvic floor. By offering detailed insight into each of these areas, this article aims to provide a comprehensive guide on contemporary assessment and treatment options to address pelvic floor imbalances. In the following paragraph, we'll begin by examining the state-of-the-art tools to accurately diagnose pelvic floor dysfunction.
Professional Diagnostic Tools for Pelvic Floor disfunction
Professional Diagnostic Tools for Pelvic Floor Dysfunction An integral part of the assessment and treatment options for pelvic floor imbalances revolves around the use of advanced, professional diagnostic tools. These precise instruments allow medical professionals to accurately determine whether a pelvic floor is tight, weak, or experiencing other imbalance issues. Essentially, these tools act as investigative aids, enabling doctors to diagnose and subsequently treat pelvic floor dysfunctions effectively. Diagnostic tools vary widely, each offering unique perspectives to accurately evaluate the state of the pelvic floor. For instance, physical examinations remain consistently effective as the primary step. A well-trained healthcare provider can gather essential information about pelvic floor muscle strength and endurance, coordination, and potential existence of trigger points and organ prolapse through touch. However, for more complex or intricate diagnostic measures, various sophisticated tools are employed. One of the state-of-the-art diagnostic tools is electromyography (EMG). This technique involves measuring the electrical activity of muscles when they are at rest and when they contract. For the pelvic floor, EMG can prove invaluable, as it helps track muscle tension, responsiveness, and identify any potential nerve complications that might be enhancing the dysfunction. Another remarkable tool aiding in pelvic floor dysfunction diagnosis is ultrasound imaging. This non-invasive approach allows professionals to visually assess the functionality of pelvic floor muscles. Ultrasound grants a real-time image of muscle contraction and relaxation patterns, assisting professionals in identifying abnormal movements and deducing the best possible therapeutic measures. Additionally, diagnostic tools also include manometry tests that evaluate muscle strength in the anus and rectum areas. This tool is particularly helpful in diagnosing weaknesses in the pelvic floor muscles that might lead to conditions like incontinence or constipation. When professionally administered, these diagnostic tools not only facilitate an accurate diagnosis but also enable a more personalized treatment plan. As awareness about pelvic floor disorders grows, continued advancements in these diagnostic devices are pivotal for improved patient outcomes. By employing these tools and understanding the dynamics of the pelvic floor, medical practitioners can effectively map the route towards a balanced pelvic floor and enhanced overall health. Through precise diagnostic procedures, patient education, and targeted treatment plans, it becomes possible to manage and potentially reverse pelvic floor dysfunction, taking us a step closer to a future with more assured pelvic health.
Balancing a Tight Pelvic Floor: Therapeutic Approaches
Balancing a Tight Pelvic Floor: Therapeutic Approaches In the journey towards achieving pelvic floor health, one critical area usually overlooked is ensuring the balance of a tight pelvic floor through therapeutic approaches. Generally, a pelvic floor could either be too weak, leading to incontinence, or too tight, resulting in discomfort, pain, and an array of complications. When pelvic floor muscles are too tight, they can cause conditions such as constipation, dyspareunia, urgency and frequency of urination, and pelvic pain that can interfere with the daily quality of life. Various therapeutic approaches come in handy to help balance a tight pelvic floor. Physical therapies offered by knowledgeable physiotherapists are among the essential treatment options. These can combine myofascial release, trigger point therapy, and spreading techniques designed to stretch and relax the pelvic floor muscles. This approach can address any trigger points that have developed as a result of sustained muscle tightness. Biofeedback is another effective therapeutic method that aids patients visually understand what’s happening within their bodies. Meanwhile, learning tailored relaxation exercises and stretches can educate patients on how to voluntarily relax their pelvic floor muscles, promoting healing and comfort. Cognitive-behavioral therapy can also be incredibly beneficial, helping to address the mind-body connection, particularly when the tightness is related to emotional stress or trauma. It isn’t uncommon for healthcare providers to combine different methods to get the optimal results; the strategy often depends on the specific needs and circumstances of the patient. Pelvic health physicians might also suggest medications or Botox injections as a temporary solution to aid muscle relaxation. However, it’s noteworthy that medications are rarely a long-term solution. Adopting a holistic approach is paramount. More than just the physical aspect, lifestyle adjustments can significantly aid in managing a tight pelvic floor. Elements like diet, exercise regime, stress management, and awareness of the correct posture and body mechanics play a crucial part in comprehensive treatment and preventative plans. In conclusion, therapeutic approaches for a tight pelvic floor aim to restore balance, relieve discomfort, and allow patients to regain control over their pelvic floor muscles. They are typically part of a broader treatment plan in addressing pelvic floor imbalances and should always be undertaken with the guidance of a health professional knowledgeable about pelvic health. Together, these therapeutic approaches provide valuable tools for managing and rectifying pelvic health issues, leading to a vastly improved quality of life.
Strengthening a Weak Pelvic Floor: Effective Exercises
Strengthening a weak pelvic floor is a critical, often overlooked aspect of overall health and well-being. A weak pelvic floor can be the source of embarrassing issues like incontinence, as well as contribute to serious health problems like prolapse. Thankfully, there are several effective exercises that can improve the strength and control of your pelvic floor muscles. Pelvic tilts are one of the simplest yet effective exercises for pelvic floor strengthening. They promote better control and flexibility in the region while enhancing lower back health. To perform a pelvic tilt, lie flat on your back, bend your knees, and keep your feet hip-width apart. Gently arch your lower back and then flatten it into the floor, feeling the movement in your pelvis as you rotate it slightly upward then downward. Another highly recommended exercise is the bridge. This harmonic motion targets not only the pelvic floor but also engages the glutes and lower back muscles, promoting better posture and pelvic alignment. Like with the pelvic tilt, you start in a supine position with knees bent. Then you lift your hips off the floor, creating a straight line from your shoulders to your knees. Hold the position for a few seconds before slowly lowering your body back to the initial state. Kegels, or pelvic floor contractions, are perhaps the most well-known and crucial exercise for pelvic floor strengthening. To perform a Kegel correctly, squeeze your pelvic floor muscles - the ones you use when you try to stop urinating. Hold the squeeze for ten seconds, then release for another ten. Repeat several times a day. It's pivotal to note that consistency is key when it comes to these exercises. Having a daily routine and sticking to it will yield the best results in strengthening a weak pelvic floor. Also, remember that any new exercise regime should be undertaken with caution; always consult with a healthcare professional for guidance based on individual health circumstances. Overall, through regular practice of these targeted exercises, individuals can significantly minimize the negative effects of a weak pelvic floor, and potentially prevent future health complications. Pelvic floor exercises are a practical, low-cost solution that supports long-term health and balance in the body, knitting perfectly into the basket of assessment and treatment options for pelvic floor imbalances.