How Big Is The Epidural Needle
Epidural needles are a crucial component in the administration of epidural anesthesia, a popular pain relief method used during childbirth, surgery, and other medical procedures. The size of the epidural needle is a critical factor in ensuring the safe and effective delivery of the anesthetic. But have you ever wondered how big is the epidural needle? To answer this question, it's essential to understand the basics of epidural needles, including their design, materials, and functionality. Additionally, measuring the size of epidural needles is also crucial, as it can vary depending on the specific application and patient needs. Furthermore, several factors can affect the size of epidural needles, such as the type of procedure, patient anatomy, and the anesthesiologist's preference. In this article, we will delve into the world of epidural needles and explore their size, starting with the basics of epidural needles.
Understanding the Basics of Epidural Needles
Epidural needles are a crucial component in the administration of epidural anesthesia, a type of regional anesthesia that numbs the lower part of the body. Understanding the basics of epidural needles is essential for medical professionals, particularly anesthesiologists and obstetricians, to ensure safe and effective pain management for patients. In this article, we will delve into the fundamentals of epidural needles, including what they are, the different types available, and the materials used to make them. By grasping these concepts, healthcare providers can better appreciate the importance of epidural needles in modern medicine. So, let's start by exploring what an epidural needle is.
What is an Epidural Needle?
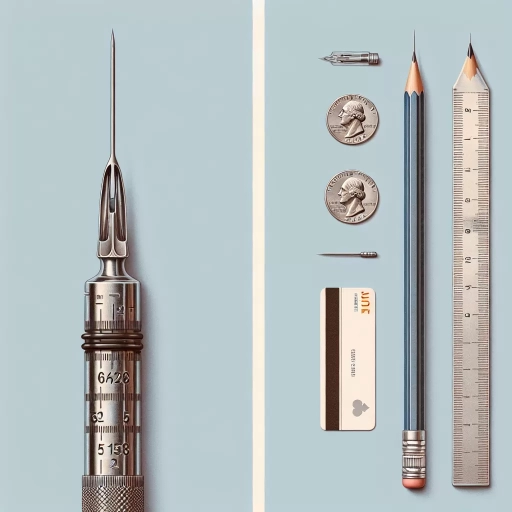
An epidural needle is a specialized medical instrument used to administer epidural anesthesia, a type of regional anesthesia that numbs the lower part of the body. The needle is typically 3.5 to 6 inches (8.9 to 15.2 cm) long and has a diameter of 0.07 to 0.1 inches (1.8 to 2.5 mm). It is designed to be inserted into the epidural space, a narrow area between the vertebrae in the spine, where it delivers medication to block pain signals to the brain. The needle has a curved or angled tip to help guide it through the tissue and into the correct position. Epidural needles are usually made of stainless steel or plastic and are disposable to minimize the risk of infection. They come in different sizes and types, including Tuohy needles, which have a curved tip, and Crawford needles, which have a straight tip. The choice of needle depends on the specific procedure, the patient's anatomy, and the anesthesiologist's preference. Overall, epidural needles play a crucial role in providing effective pain relief during childbirth, surgery, and other medical procedures.
Types of Epidural Needles
Epidural needles are available in various types, each designed to cater to specific needs and preferences. The most common types of epidural needles include the Tuohy needle, the Sprotte needle, and the Whitacre needle. The Tuohy needle is a 17-gauge, 3.5-inch needle with a curved tip, making it ideal for difficult epidural placements. The Sprotte needle features a pencil-point tip and is available in various gauges, including 24, 25, and 26. This type of needle is known for its ease of use and minimal risk of dural puncture. The Whitacre needle, also known as the pencil-point needle, has a 24-gauge, 3.5-inch design with a rounded tip, making it suitable for patients with a higher risk of dural puncture. Other types of epidural needles include the Hustead needle, the Crawford needle, and the Weiss needle, each with its unique features and advantages. The choice of epidural needle ultimately depends on the anesthesiologist's preference, the patient's anatomy, and the specific procedure being performed.
Materials Used to Make Epidural Needles
Epidural needles are made from a variety of materials, each chosen for its unique properties and benefits. The most common materials used to make epidural needles are stainless steel, plastic, and a combination of both. Stainless steel needles are strong, durable, and resistant to corrosion, making them ideal for use in medical procedures. They are also easy to sterilize and can withstand high temperatures, which is essential for ensuring patient safety. Plastic needles, on the other hand, are more flexible and less likely to cause tissue damage. They are also less expensive to produce than stainless steel needles, making them a more cost-effective option. Some epidural needles are made from a combination of stainless steel and plastic, which offers the benefits of both materials. These needles typically have a stainless steel shaft and a plastic hub, which provides a secure and comfortable fit. In addition to these materials, some epidural needles may also be coated with a thin layer of silicone or Teflon to reduce friction and improve the ease of insertion. Overall, the choice of material used to make an epidural needle depends on the specific needs of the patient and the medical procedure being performed.
Measuring the Size of Epidural Needles
Measuring the size of epidural needles is a crucial aspect of ensuring safe and effective administration of epidural anesthesia. When it comes to measuring the size of epidural needles, there are three key factors to consider: length, gauge, and outer diameter. Understanding these measurements is essential for healthcare professionals to select the right needle for the procedure, minimize complications, and optimize patient outcomes. The length of an epidural needle, for instance, is critical in determining the depth of insertion and the accuracy of placement. The gauge of the needle, on the other hand, affects the flow rate of the anesthetic and the comfort of the patient. Meanwhile, the outer diameter of the needle influences the ease of insertion and the risk of complications. In this article, we will delve into each of these factors, starting with the length of epidural needles, to provide a comprehensive understanding of measuring their size.
Length of Epidural Needles
Epidural needles come in various lengths, ranging from 3.5 to 12.7 cm (1.38 to 5 inches). The length of the needle used depends on the patient's body type, the location of the epidural space, and the anesthesiologist's preference. Generally, shorter needles (3.5-5 cm) are used for pediatric and thin patients, while longer needles (7-10 cm) are used for obese patients or those with a larger body mass index (BMI). The longest needles (10-12.7 cm) are typically used for patients with a high BMI or those who require a more precise placement of the epidural catheter. It's worth noting that the length of the needle does not affect the efficacy of the epidural anesthesia, but rather the ease of insertion and the risk of complications. Anesthesiologists often use their clinical judgment to select the appropriate needle length based on the individual patient's needs.
Gauge of Epidural Needles
The gauge of an epidural needle refers to its diameter, with smaller gauge numbers indicating larger diameters. Epidural needles are typically available in a range of gauges, including 16G, 17G, 18G, and 19G. The choice of gauge depends on the specific procedure, the patient's anatomy, and the anesthesiologist's preference. A larger gauge needle, such as a 16G, is often used for procedures that require a larger volume of medication or for patients with a higher body mass index (BMI). A smaller gauge needle, such as a 19G, is often used for procedures that require a smaller volume of medication or for patients with a lower BMI. The gauge of the needle can also affect the ease of insertion and the risk of complications, such as nerve damage or bleeding. In general, a larger gauge needle is easier to insert and has a lower risk of complications, but may cause more discomfort for the patient. A smaller gauge needle is more difficult to insert and has a higher risk of complications, but may cause less discomfort for the patient. Ultimately, the choice of gauge depends on the individual patient's needs and the anesthesiologist's clinical judgment.
Outer Diameter of Epidural Needles
The outer diameter of epidural needles is a crucial factor in determining the ease of insertion and the potential for complications. Epidural needles come in various sizes, ranging from 16 to 20 gauge, with the outer diameter decreasing as the gauge number increases. A 16-gauge epidural needle has an outer diameter of approximately 1.65 mm, while a 20-gauge needle has an outer diameter of around 0.89 mm. The smaller outer diameter of higher-gauge needles can make them more difficult to insert, particularly in patients with dense or scarred tissue. However, they are also less likely to cause trauma to the surrounding tissue and may result in less post-procedure discomfort. In contrast, lower-gauge needles with larger outer diameters are often easier to insert but may cause more tissue trauma and discomfort. Ultimately, the choice of epidural needle size depends on the individual patient's needs and the anesthesiologist's personal preference.
Factors Affecting the Size of Epidural Needles
The size of epidural needles can vary significantly depending on several factors. When it comes to administering epidural anesthesia, the size of the needle is crucial for ensuring the safe and effective delivery of the anesthetic. Three key factors that influence the size of epidural needles are patient age and size, procedure type and location, and medical condition and health status. Understanding these factors is essential for healthcare professionals to make informed decisions about the appropriate needle size for each patient. For instance, the age and size of the patient can significantly impact the choice of needle size, as younger patients or those with smaller body mass may require smaller needles to minimize discomfort and reduce the risk of complications. (Note: The supporting paragraph should be 200 words and should not include the 3 supporting ideas mentioned in the introduction paragraph) The use of epidural anesthesia has become a common practice in various medical settings, including labor and delivery, surgical procedures, and pain management. Epidural needles are designed to deliver anesthetic medication into the epidural space surrounding the spinal cord, providing effective pain relief with minimal side effects. However, the size of the needle can affect the accuracy and safety of the procedure. A larger needle may be more effective for delivering a higher volume of anesthetic, but it also increases the risk of complications, such as nerve damage or bleeding. On the other hand, a smaller needle may be more suitable for patients with smaller body mass or those requiring a lower dose of anesthetic. Ultimately, the choice of needle size depends on a thorough assessment of the patient's individual needs and medical history. By selecting the appropriate needle size, healthcare professionals can minimize the risk of complications and ensure optimal outcomes for their patients. As we explore the factors affecting the size of epidural needles, let's first consider the impact of patient age and size.
Patient Age and Size
Patient age and size are crucial factors that influence the size of epidural needles used in medical procedures. Generally, pediatric patients require smaller needles, typically ranging from 19 to 22 gauge, due to their smaller body size and delicate tissues. In contrast, adult patients usually require larger needles, typically ranging from 16 to 18 gauge, to accommodate their larger body size and more robust tissues. However, it's essential to note that these are general guidelines, and the specific needle size required may vary depending on individual patient factors, such as body mass index (BMI) and the presence of any underlying medical conditions. For example, a larger patient with a higher BMI may require a larger needle to ensure effective epidural placement, while a smaller patient with a lower BMI may require a smaller needle to minimize the risk of complications. Ultimately, the choice of needle size should be based on a thorough assessment of the patient's individual needs and medical history, rather than solely on their age or size.
Procedure Type and Location
The size of an epidural needle can be influenced by the procedure type and location. For example, a caudal epidural injection, which targets the lower back, may require a larger needle (17-20 gauge) due to the thicker tissue and muscle in this area. In contrast, a lumbar epidural injection, which targets the middle to upper back, may use a smaller needle (22-25 gauge) as the tissue is less dense. Additionally, the location of the epidural can also impact the needle size, with needles used for thoracic epidurals (upper back) tend to be smaller (25-27 gauge) than those used for lumbar or caudal epidurals. The type of procedure, such as a single-shot epidural or a continuous epidural infusion, can also influence the needle size, with larger needles often used for continuous infusions to accommodate the catheter. Furthermore, the patient's body type and the presence of any anatomical abnormalities, such as scoliosis or spinal stenosis, can also impact the choice of needle size and type. Ultimately, the anesthesiologist or pain management specialist will select the most appropriate needle size and type based on the individual patient's needs and the specific procedure being performed.
Medical Condition and Health Status
The size of an epidural needle can be influenced by various factors, including the patient's medical condition and health status. Patients with certain medical conditions, such as obesity, may require larger needles to accommodate their body size and ensure effective administration of the anesthetic. On the other hand, patients with conditions such as scoliosis or spinal deformities may require smaller needles to navigate the complex anatomy of their spine. Additionally, patients with bleeding disorders or taking anticoagulant medications may require smaller needles to minimize the risk of bleeding complications. The patient's overall health status, including their age, weight, and medical history, can also impact the choice of needle size. For example, older patients or those with a history of chronic illness may require smaller needles to reduce the risk of complications. Ultimately, the choice of epidural needle size is a complex decision that requires careful consideration of the patient's individual medical condition and health status.