How Long Does Tylenol 3 Stay In Your System
Tylenol 3, a prescription pain reliever containing codeine and acetaminophen, is commonly used to treat moderate to severe pain. However, its presence in the system can be a concern for individuals who need to undergo drug testing or are worried about potential interactions with other medications. The duration of Tylenol 3 in the system depends on various factors, including the individual's metabolism, dosage, and frequency of use. Understanding how Tylenol 3 is processed and eliminated by the body is also crucial in determining its stay in the system. Additionally, knowing how Tylenol 3 is tested for in the system can provide valuable insights. In this article, we will explore the factors that affect the duration of Tylenol 3 in the system, how it is processed and eliminated, and how it is tested for. First, let's examine the factors that influence how long Tylenol 3 stays in the system.
Factors Affecting the Duration of Tylenol 3 in the System
The duration of Tylenol 3 in the system can vary significantly from person to person, influenced by several key factors. Understanding these factors is crucial for safe and effective use of this medication. Three primary factors that affect how long Tylenol 3 stays in the system are metabolic rate and body composition, age and overall health, and dosage and frequency of use. Each of these factors plays a significant role in determining the half-life of Tylenol 3, which is the time it takes for the body to eliminate half of the drug. For instance, individuals with a higher metabolic rate may process Tylenol 3 more quickly, reducing its duration in the system. Similarly, the age and overall health of a person can impact the efficiency of their body's drug elimination processes. The dosage and frequency of Tylenol 3 use also directly influence how long the drug remains active in the body. By understanding these factors, individuals can better manage their medication regimen. Starting with the most immediate influence, metabolic rate and body composition are key determinants in how quickly Tylenol 3 is metabolized and eliminated from the body.
Metabolic Rate and Body Composition
Metabolic rate and body composition play a significant role in determining how long Tylenol 3 stays in the system. Metabolic rate refers to the rate at which the body burns calories to produce energy, and it can vary significantly from person to person. Individuals with a faster metabolic rate tend to process and eliminate substances, including medications like Tylenol 3, more quickly. On the other hand, those with a slower metabolic rate may take longer to eliminate the medication, leading to a longer duration of action. Body composition also affects the duration of Tylenol 3 in the system. People with a higher percentage of body fat may experience a longer duration of action, as the medication is stored in fatty tissues and released slowly into the bloodstream. Conversely, individuals with a leaner body composition may experience a shorter duration of action, as the medication is eliminated more quickly. Additionally, factors such as age, sex, and overall health can also influence metabolic rate and body composition, which in turn affect the duration of Tylenol 3 in the system. For example, older adults may have a slower metabolic rate and a higher percentage of body fat, leading to a longer duration of action. Similarly, individuals with certain medical conditions, such as liver or kidney disease, may experience altered metabolic rates and body composition, affecting the duration of Tylenol 3 in the system. Overall, understanding the interplay between metabolic rate, body composition, and other factors is essential for predicting how long Tylenol 3 will stay in the system.
Age and Overall Health
Age is a significant factor in determining overall health, and it plays a crucial role in how the body processes medications like Tylenol 3. As people age, their bodies undergo natural changes that can affect the way they metabolize and eliminate drugs. Older adults may experience a decline in liver function, which can lead to slower metabolism and increased levels of Tylenol 3 in the system. Additionally, age-related changes in kidney function can impair the body's ability to excrete the drug, causing it to stay in the system for longer periods. Furthermore, older adults may be more likely to have underlying health conditions, such as liver or kidney disease, that can impact the duration of Tylenol 3 in the system. As a result, older adults may need to take lower doses or have their medication adjusted to avoid adverse effects. On the other hand, younger individuals tend to have faster metabolism and better organ function, which can lead to faster elimination of Tylenol 3 from the system. However, it's essential to note that individual factors, such as overall health, body composition, and genetics, can influence the duration of Tylenol 3 in the system, regardless of age.
Dosage and Frequency of Use
The dosage and frequency of use of Tylenol 3 can significantly impact how long it stays in the system. The standard dosage of Tylenol 3 is 1-2 tablets every 4-6 hours as needed, not to exceed 8 tablets in 24 hours. Taking more than the recommended dose or taking it more frequently can lead to a longer duration of the medication in the system. For example, taking 2 tablets every 4 hours will result in a longer duration than taking 1 tablet every 6 hours. Additionally, taking Tylenol 3 for an extended period can lead to accumulation of the medication in the body, resulting in a longer duration of action. It is essential to follow the recommended dosage and frequency of use to avoid prolonged exposure to the medication. Furthermore, individuals with liver or kidney disease may need to adjust their dosage and frequency of use to avoid accumulation of the medication, which can lead to adverse effects.
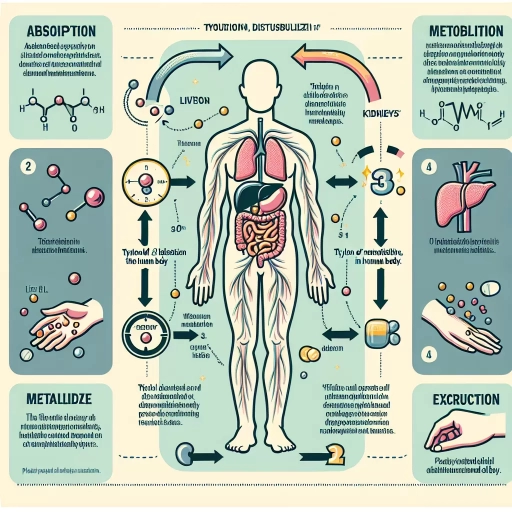
How Tylenol 3 is Processed and Eliminated by the Body
Here is the introduction paragraph: When it comes to managing pain, Tylenol 3 is a commonly prescribed medication that combines acetaminophen and codeine. But have you ever wondered how this medication is processed and eliminated by the body? Understanding the journey of Tylenol 3 from ingestion to excretion can provide valuable insights into its effectiveness and potential side effects. The process involves several key steps, including absorption and distribution in the body, metabolism by the liver and excretion by the kidneys, and the concept of half-life and peak concentration. In this article, we will delve into each of these stages, starting with how Tylenol 3 is absorbed and distributed throughout the body.
Absorption and Distribution in the Body
After ingestion, Tylenol 3 is absorbed into the bloodstream through the gastrointestinal tract, primarily in the small intestine. The absorption rate is influenced by factors such as the presence of food, the dosage form, and individual variations in gut motility and pH. Once absorbed, the acetaminophen and codeine components of Tylenol 3 are distributed throughout the body via the bloodstream. Acetaminophen is widely distributed, with high concentrations found in the liver, kidneys, and brain, while codeine is primarily distributed to the liver, lungs, and brain. The distribution of these components is influenced by their lipophilicity, protein binding, and the presence of specific transporters. The liver plays a crucial role in the distribution of Tylenol 3, as it is the primary site for the metabolism of both acetaminophen and codeine. The liver's metabolic processes, including glucuronidation and sulfation, convert these components into more water-soluble metabolites, which are then excreted in the urine. The distribution of Tylenol 3 is also influenced by the body's pH levels, with the components being more lipophilic in acidic environments and more hydrophilic in basic environments. This affects their ability to cross cell membranes and interact with specific receptors. Overall, the absorption and distribution of Tylenol 3 are complex processes that involve multiple factors and pathways, ultimately influencing the drug's efficacy and potential for adverse effects.
Metabolism by the Liver and Excretion by the Kidneys
The liver and kidneys play crucial roles in the metabolism and excretion of Tylenol 3. The liver is responsible for metabolizing the acetaminophen component of Tylenol 3, converting it into a compound that can be easily eliminated from the body. This process involves the cytochrome P450 enzyme system, which breaks down the acetaminophen into its metabolites. The liver also metabolizes the codeine component of Tylenol 3, converting it into morphine, which is then further metabolized into its own set of metabolites. The kidneys, on the other hand, are responsible for excreting the metabolites of both acetaminophen and codeine from the body. They filter the blood and remove the waste products, which are then excreted in the urine. The kidneys also play a role in regulating the amount of Tylenol 3 in the body by adjusting the rate of excretion based on factors such as hydration levels and overall kidney function. Overall, the liver and kidneys work together to efficiently metabolize and eliminate Tylenol 3 from the body, with the liver breaking down the medication into its metabolites and the kidneys excreting those metabolites in the urine.
Half-Life and Peak Concentration
The half-life and peak concentration of Tylenol 3, also known as acetaminophen with codeine, are crucial factors in understanding how the medication is processed and eliminated by the body. The half-life of a drug refers to the time it takes for the concentration of the medication in the bloodstream to reduce by half. For Tylenol 3, the half-life of acetaminophen is approximately 2-3 hours, while the half-life of codeine is around 2.5-3 hours. This means that it takes around 10-15 hours for the body to eliminate 99% of the acetaminophen and codeine from the system. The peak concentration of Tylenol 3, on the other hand, refers to the highest level of the medication in the bloodstream, which typically occurs within 1-2 hours after ingestion. At this point, the medication is at its most potent, providing maximum pain relief. As the medication is metabolized and eliminated, the concentration in the bloodstream decreases, and the pain-relieving effects begin to wear off. Understanding the half-life and peak concentration of Tylenol 3 is essential for determining the optimal dosage and frequency of administration to achieve effective pain management while minimizing the risk of adverse effects.
Testing for Tylenol 3 in the System
Testing for Tylenol 3 in the system is a crucial process, especially in medical and legal settings. Tylenol 3, also known as acetaminophen with codeine, is a prescription medication used to relieve moderate to severe pain. However, its misuse can lead to addiction and other health complications. When it comes to testing for Tylenol 3, there are several factors to consider, including the types of drug tests and their sensitivity, the window of detection for the substance, and the potential for false positives and interfering substances. Understanding these aspects is essential for accurate and reliable test results. In this article, we will delve into the world of drug testing for Tylenol 3, starting with the various types of drug tests and their sensitivity, which play a critical role in detecting the presence of this medication in the system.
Types of Drug Tests and Their Sensitivity
There are several types of drug tests, each with varying levels of sensitivity. The most common types of drug tests include urine tests, blood tests, saliva tests, and hair tests. Urine tests are the most widely used and can detect the presence of Tylenol 3 in the system for up to 3 days after the last use. Blood tests are more sensitive and can detect the presence of Tylenol 3 for up to 12 hours after the last use. Saliva tests can detect the presence of Tylenol 3 for up to 2 days after the last use. Hair tests are the most sensitive and can detect the presence of Tylenol 3 for up to 90 days after the last use. It's worth noting that the sensitivity of these tests can vary depending on the individual's metabolism, the amount of Tylenol 3 consumed, and the frequency of use. Additionally, some tests may be more sensitive to certain components of Tylenol 3, such as codeine or acetaminophen, than others. Overall, the type of test used and its sensitivity can impact the accuracy of the results and the length of time that Tylenol 3 can be detected in the system.
Window of Detection for Tylenol 3
The window of detection for Tylenol 3, which contains a combination of acetaminophen and codeine, varies depending on the testing method and individual factors. In general, codeine can be detected in the system for several days after the last dose. Here's a breakdown of the typical detection windows for Tylenol 3: * **Urine tests:** Codeine can be detected in urine for 2-4 days after the last dose, with peak concentrations occurring within 2-6 hours after ingestion. However, some studies suggest that codeine can be detectable in urine for up to 7-10 days in heavy users. * **Blood tests:** Codeine can be detected in blood for 12-24 hours after the last dose, with peak concentrations occurring within 1-2 hours after ingestion. * **Saliva tests:** Codeine can be detected in saliva for 1-4 days after the last dose, with peak concentrations occurring within 1-2 hours after ingestion. * **Hair tests:** Codeine can be detected in hair for several months after the last dose, with a typical detection window of 90 days. However, this method is not commonly used for detecting Tylenol 3 use. It's essential to note that these detection windows can vary depending on individual factors, such as the dose and frequency of Tylenol 3 use, metabolism, and overall health. Additionally, some testing methods may be more sensitive than others, which can affect the detection window. If you're concerned about testing for Tylenol 3 in your system, it's best to consult with a medical professional or a qualified testing expert.
False Positives and Interfering Substances
False positives and interfering substances can significantly impact the accuracy of Tylenol 3 tests. A false positive occurs when a test incorrectly identifies the presence of a substance, in this case, codeine or acetaminophen, when it is not actually present. This can happen due to various factors, including the presence of certain medications, foods, or substances that can interfere with the test results. For instance, certain antibiotics, such as rifampicin, and anticonvulsants, like carbamazepine, can cause false positives for codeine. Similarly, consuming poppy seeds or certain herbal supplements can also lead to false positives. Interfering substances can also affect the accuracy of test results. For example, high levels of bilirubin, a compound produced during the breakdown of red blood cells, can interfere with the detection of acetaminophen. Additionally, certain medical conditions, such as liver or kidney disease, can also impact the accuracy of test results. It is essential to consider these factors when interpreting test results to ensure accurate and reliable detection of Tylenol 3 in the system.