How Long For Ozempic To Work
 To comprehend the efficiency and effectiveness of any medication, a patient must exhibit patience and understanding—Ozempic, used to manage type 2 diabetes, is no exception. In this article, we unravel the truth behind the timeframe in which Ozempic operates and its underlying operational mechanics. In our first segment, 'Understanding Ozempic and its functionality,' we delve into the complexity of this innovative medicine and how it functions within the mechanics of our body. Next, we navigate the course of action in 'Assessing the timeline: When will Ozempic start to work?' enabling us to map out the timeframe required to experience the medication's effectiveness. Lastly, but most crucially, we provide guidance on how to reinforce the medication's efficacy with lifestyle changes in 'Optimizing Ozempic effectiveness with lifestyle modifications.' Each piece of information is meticulously curated to serve as your comprehensive guide to getting the best out of Ozempic. Without further ado, let us embark on this journey of understanding Ozempic and its functionalities.
To comprehend the efficiency and effectiveness of any medication, a patient must exhibit patience and understanding—Ozempic, used to manage type 2 diabetes, is no exception. In this article, we unravel the truth behind the timeframe in which Ozempic operates and its underlying operational mechanics. In our first segment, 'Understanding Ozempic and its functionality,' we delve into the complexity of this innovative medicine and how it functions within the mechanics of our body. Next, we navigate the course of action in 'Assessing the timeline: When will Ozempic start to work?' enabling us to map out the timeframe required to experience the medication's effectiveness. Lastly, but most crucially, we provide guidance on how to reinforce the medication's efficacy with lifestyle changes in 'Optimizing Ozempic effectiveness with lifestyle modifications.' Each piece of information is meticulously curated to serve as your comprehensive guide to getting the best out of Ozempic. Without further ado, let us embark on this journey of understanding Ozempic and its functionalities.Understanding Ozempic and its functionality
Ozempic is a revolutionary medicinal advancement in the realm of diabetes maintenance. Incorporating an advanced formulation, it has transformed the way our body's sugar level is managed. To effectively comprehend the true value of Ozempic, we must examine the foundational details that make this medication so exceptional. First, we must delve into the science behind Ozempic, which illuminates why it's effective in controlling glucose levels. Following that, a precise understanding of how Ozempic functions within the human body is necessary, reaffirming its importance in effectively combating rollercoaster sugar levels. Finally, to implement this medication continually and efficiently, it's vital to recognize the variables that can sway Ozempic's absorption rate in the body. Understanding these aspects helps individuals manage their health conditions more effectively and bolsters their confidence in the treatment. The science behind Ozempic unfolds an intriguing story of medical innovation, moving us closer to more effective diabetes management techniques. So, let's unfold this story beginning with the science underlying Ozempic's formulation and efficacy.
The science behind Ozempic
Ozempic, a medication designed for the management of type 2 diabetes, has caught the attention of the medical world due to its innovation and efficiency. The science behind Ozempic lies in its specialized formulation which was developed based on advanced medical research and technology. Ozempic, or semaglutide, is a glucagon-like peptide-1 (GLP-1) receptor agonist that mimics the function of the body's native GLP-1. This hormone plays a critical role in the regulation of glucose levels in the body. It stimulates insulin production in response to high glucose levels, helps in suppressing the release of glucagon (a hormone that increases glucose levels), and aids in slowing down gastric emptying. By imitating these actions of native GLP-1, Ozempic provides an enhanced control over blood sugar levels. Additionally, Ozempic exhibits an incredible degree of durability and longevity in the body. It has a half-life of approximately one week which enables once-weekly dosing - a convenience not common among diabetes medications. This is a result of semaglutide's structural similarity to native GLP-1, with minor modifications to make it resistant to degradation by the enzyme called dipeptidyl peptidase-4, which breaks down naturally-occurring GLP-1 in the body. Moreover, a surprising characteristic of Ozempic, which sets it apart from most diabetes medications, is its potential in inducing weight loss. This is primarily due to the drug's effect of slowing down gastric emptying, causing patients to feel satiated and curbing their appetite. Some studies have shown patients losing a significant amount of weight over several weeks of taking this medication. Based on these mechanisms, it is clear that the power of Ozempic lies in its multi-faceted approach to managing diabetes. It not only regulates blood glucose levels effectively but also addresses auxiliary issues connected to the disease, such as obesity. Understanding the science behind Ozempic and its functionality is a firm step in understanding how it takes time for Ozempic to work, generally starting to lower blood sugar levels within a week of the first dose and reaching maximum effect after 5-7 weeks. However, its groundbreaking effects on weight loss may take longer to manifest. The understanding of this advanced drug, Ozempic, reflects the progress that medical science has made in managing chronic diseases like diabetes, opening up new avenues for more efficient and user-friendly modes of treatment.
How Ozempic operates in the body
Ozempic, known by the generic name Semaglutide, operates in the body by imitating the function of a natural hormone, glucagon-like-peptide-1 (GLP-1), which is typically released into the bloodstream after a meal. Serving as a powerful controller of the body's metabolism, GLP-1 primarily works by stimulating the production of insulin, suppressing the release of glucagon, and slowing gastric emptying, which sequentially lowers blood glucose levels. Ozempic, when administered, adheres to the same GLP-1 receptors, thereby achieving similar functions. A noticeable uniqueness is that Ozempic has a longer-lasting effect compared to the natural hormone, remaining in the body for up to one week, consequently providing a prolonged and steady regulation of blood glucose. Moreover, Ozempic slows down the speed at which food moves through the stomach. This process helps control the influx of sugar into the bloodstream, preventing any sudden spikes or dips in blood sugar levels post meals. Slowing down the gastric emptying also induces a feeling of satiety, which may contribute to weight loss, a common secondary benefit reported by users. The stimulation of insulin and suppression of glucagon by Ozempic are also pivotal in maintaining glycaemic control. This is because when there is excess glucose in the blood, insulin allows for this surplus sugar to be utilized by the body's cells, hence, reducing blood glucose concentration. In contrast, glucagon has the opposite effect, increasing blood glucose levels by mobilizing stored glucose when levels are low. By stimulating insulin production and inhibiting glucagon, Ozempic works to create a balance, ensuring blood sugar levels remain within the healthy range. Finally, it's worth noting that even though Ozempic has the ability to change how the body processes sugar, it does not cause the body to overproduce insulin, thereby, safeguarding users against suffering hypoglycemia – a significant risk associated with some other diabetes medications. Therefore, the mechanism of Ozempic not just revolves around its impact on insulin and glucagon but also involves effectively balancing blood glucose levels, aiding weight loss, and minimizing potential side effects. In summary, the functionality of Ozempic in the body is two-pronged – it imitates the actions of the naturally occurring hormone, GLP-1, while introducing long-lasting effects to help patients achieve better blood glucose control and possible weight loss.
The factors that affect Ozempic's absorption rate
There are several factors that influence how Ozempic (Semaglutide), a glucagon-like peptide-1 (GLP-1) agonist, is absorbed into the body, which subsequently determines the duration before its effects become noticeable. One primary influence is the manner of administration. Ozempic is injected subcutaneously, typically once a week, which allows it to slowly seep into the bloodstream over a prolonged period, enabling a steady release and consistent action. The physiological characteristics of the individual are also crucial. Body weight, metabolic rate, and general health conditions can influence how Ozempic is absorbed. Furthermore, the drug's bioavailability, which refers to the proportion of the drug that enters the circulation when introduced into the body and is able to have an active effect, differs from person to person due to variables like genetic factors, age, and gender. The presence or absence of food in the stomach affects the absorption rate too. While Ozempic is designed to be taken without regards to meals, it may work differently in an empty stomach versus a full one, primarily because of the various metabolic and enzymatic activities. Medication interactions can also alter the absorption, as certain drugs might either speed up or slow down its metabolization or potentially affect its pathway, causing Ozempic to work faster or slower. It is recommended that individuals discuss all medications and supplements they are currently taking with their healthcare provider before starting Ozempic to prevent adverse interactions. Overall, the factors influencing Ozempic's absorption rate and the lengthy process from administration to effect highlight the complexity of this medication's function within the body. By understanding these nuances, healthcare providers and patients can make more informed decisions about starting, maintaining or adjusting the dosage of Ozempic in their diabetes management.
Assessing the timeline: When will Ozempic start to work?
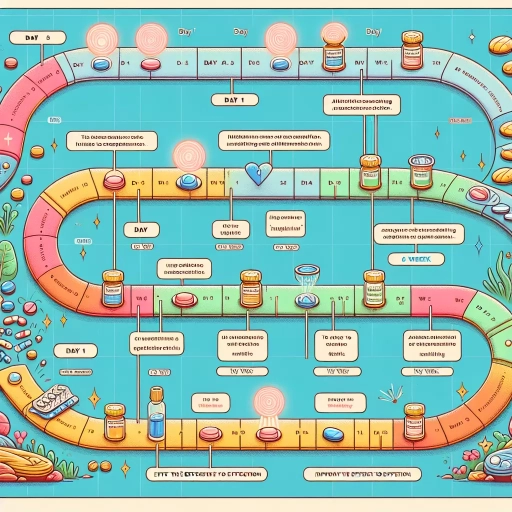
Delving into the exploration of Ozempic, a well-acclaimed diabetes drug, this article will present an in-depth analysis of its timeline to efficacy. While the story of its functionality is not as simple as taking a pill and feeling immediate change, it's a gradual process that unfolds over time. Commencing from the immediate effects post-administration, our journey spans across observing the progressive impact that Ozempic establishes over weeks to the firsthand testimonies and compelling clinical evidences that establish the drugs' efficacy timeframe. Embarking on the first leg of this journey, we will discuss the immediate effects one may experience after starting Ozempic, a critical cornerstone in understanding this drug's functional course. The timeline is key to setting realistic expectations and fostering a more effective and patience-oriented treatment process.
Immediate effects post administration
The immediate effects post-administration of Ozempic are a crucial aspect in its efficiency profile. Understanding these effects helps paint a clear picture of the drug's performance, complementing the broader timeline assessment of how long it takes for Ozempic to start working. Immediately after administration, Ozempic begins to interact with the body's endocrine system focusing on glycemic regulation. Its active ingredient, Semaglutide, mimics a naturally occurring hormone in the body termed as GLP-1 (glucagon-like peptide 1). This synthetic match stimulates insulin secretion while reducing the release of glucagon - both essential components in stimulating lower blood sugar levels. However, despite its immediate interaction with the body system, do not expect an immediate dip in blood glucose levels. The physiological effects of Ozempic, like most GLP-1 receptor agonists, accumulate gradually. While the drug starts its work on molecular level immediately, noticeable changes in blood sugar levels typically begin to appear after a few weeks of regular administration - often around week 4 to 5. Immediately post-administration, some patients may experience certain side effects. Common ones include slight nausea, reduced appetite, and occasional stomach upsets. These effects, while in most cases mild, can be considered the body's immediate response to the drug. Health care practitioners usually advise that these side effects wane over time as the body adjusts to the new medication. In conclusion, the drug's initiation in the body is not synonymous with experiencing the expected clinical outcomes immediately. The immediate post-administration effects are subtle and more body tolerance and drug functioning-centric than directly related to a steep drop in blood sugar levels. A comprehensive timeline assessment, like the one encompassing long-term effects, is necessary to fully appreciate the effectiveness of Ozempic. Thus, understanding this timeline assists one in setting realistic expectations and establishing effective diabetes management strategies.
Observing Ozempic’s progressive impact over weeks
Ozempic's progressive impact over weeks is striking, revealing a significant transformation that is both palpable and measurable. It’s not an instant remedy; the effects build gradually and reach full efficacy usually between 7 to 14 weeks. During the early stages of the treatment, patients may notice a subtle decrease in blood glucose levels. This reduction is indicative of Ozempic beginning to do its work and is the first milestone on the journey to improved health. By weeks seven to eight, many patients report weight loss as the medication helps regulate the body's insulin levels and suppresses appetite. These weight-related changes can be highly motivating and provide a beacon of hope for further positive modifications. Accessibility to healthier food choices becomes easier since the appetite is modulated, reinforcing a cycle of healthier eating and lifestyle improvements. As the treatment reaches ten weeks, more substantial effects are observed. Reduced blood sugar levels become more consistent and less sporadic, contributing to a sense of stability and control over the condition. It's around this time that patients may notice an overall enhancement in their wellbeing, with feelings of vitality emerging as a distinct contrast from their pre-treatment condition. As Ozempic continues its work beyond this timeline, its impact grows stronger. By the 14th week, most patients have reported a noteworthy reduction in their HbA1c levels, the long-term gauge of blood glucose control. This further reduction indicates that Ozempic is working optimally, helping those with type 2 diabetes manage their condition more effectively. Nevertheless, individual responses to Ozempic can vary greatly. While some may witness effects early in the timeline, others might need more time. Importantly, the final outcome is not just about the physical changes, but also about how these improvements alter individuals' health perspective, inspire healthier choices, and enrich their life quality. Observing Ozempic's progressive impact over weeks thus forms a crucial part of understanding the overall benefit of the treatment.
User testimonies and clinical evidences of Ozempic effectiveness timeframe
User testimonials and clinical evidence consistently corroborate the effectiveness of Ozempic within a specified timeframe. A multitude of users have reported noticeable changes in their blood sugar levels within 2-4 weeks of initiating this anti-diabetes medication. Furthermore, many have relayed a significant reduction in their blood sugar spikes, accompanied by weight loss, which is an additional advantage of Ozempic. Some users, though, have observed it can take up to 5-7 weeks to experience the full benefits of the medication, particularly for those with adverse initial reactions. Similarly, clinical studies affirm the efficacy of Ozempic within a few weeks. A study published in the Journal of the American Medical Association revealed that patients who took Ozempic showed a reduction in their HbA1c levels just after 12 weeks of treatment demonstrating the rapid effectiveness of this glucagon-like peptide-1 (GLP-1) receptor agonist in regulating blood glucose levels. Furthermore, a 30-week randomized, double-blind, placebo-controlled trial published in Diabetes Care, including more than 1200 participants, demonstrated that people who used Ozempic had an improvement in their blood glucose levels as early as week 4. By week 30, up to 73% of patients had reached their HbA1c goal, indicating Ozempic's potency over an extended period. Balance is vital when interpreting these testimonies and clinical results. While the majority of users and clinical trials indicate Ozempic’s effectiveness within weeks, these results can vary based on individuals' unique health conditions, starting blood sugar levels, and their body's metabolic response. Considering these testimonies and clinical evidence, it is fair to say that Ozempic's effectiveness begins to kick in rapidly but its full potential is realized over several weeks. Therefore, patience and compliance are critical for reaping its optimal benefits.
Optimizing Ozempic effectiveness with lifestyle modifications
Optimizing the effectiveness of Ozempic, a revolutionary medication for the management of type 2 diabetes, can be significantly achieved through strategic lifestyle modifications. This article aims to explore the comprehensive benefits and potential synergistic effects of diet, physical activities, and medication compliance on enhancing the influence of Ozempic. Coupling a healthy, balanced diet with Ozempic can significantly enhance drug metabolism and efficiency, leading to better disease management. Moreover, integrating adequate physical activity into a daily routine not only promotes overall health but also boosts the impact of Ozempic by regulating blood sugar levels and promoting weight loss. Lastly, strict adherence to medication schedules ensures steady drug levels in the bloodstream, making Ozempic as effective as possible. By adhering to these key lifestyle components, one can truly optimize the benefits of this groundbreaking medication. As we delve further into the article, the indispensable role of nutritious diets will be examined thoroughly in the quest to maximize the efficacy of Ozempic.
The role of diet in enhancing Ozempic's effectiveness
Understanding the role of diet in enhancing Ozempic's effectiveness remains a pivotal aspect of the whole therapy. Medical research indicates that incorporating diet changes alongside one's prescribed medication regimen is key to amplifying the therapeutic outcomes of drugs like Ozempic. This semi-glucagon like Peptide-1 (GLP-1) receptor agonist, used in the treatment of type 2 diabetes and obesity, demonstrates optimum effectiveness when supported by a healthy nutritional intake. Proper dietary modifications make an enormous difference. Consuming a well-balanced diet rich in whole foods, lean proteins, healthy fats, vegetables, and fruits ensures the body receives essential nutrients. This practice ultimately enhances the body's metabolism, allowing more effective utilization of Ozempic and possibly accelerating its onset of action. What's more, a diet low in processed foods, sugars, and unhealthy fats helps to maintain one's blood glucose levels within a healthy range. It aids to lessen the body’s glucose production and promotes slower digestion, both of which are the pharmacological effects of Ozempic. By eating healthily, individuals allow Ozempic to perform its functions more efficiently, potentially leading to better symptom control and disease management. Incorporating fiber-rich foods into your diet can slow the rate of sugar absorption in your bloodstream and reduce the risk of blood sugar spikes that Ozempic seeks to control. Also, it's worth knowing that drinking plenty of water keeps the body hydrated, aids digestion and helps in the excretion process of metabolism by-products. Besides, meal planning and mindful eating habits also contribute considerably in enhancing the effectiveness of Ozempic. Regular, balanced, and moderate meal portions prevent overeating and sudden rises in blood glucose, which in turn ensures Ozempic can most effectively regulate one's blood sugar levels and metabolism. In conclusion, understanding the profound impact of dietary habits on Ozempic's effectiveness helps to optimize the drug's potential benefits. Smart diet modifications, alongside this medication, can create a synergistic relationship that significantly boosts your body's response to Ozempic, contributing to more efficient treatment outcomes and improved health.
Leveraging physical activities to boost Ozempic's impact
Leveraging physical activities to boost the effectiveness of Ozempic is an integral complement to the medical treatment. As an innovative medication, Ozempic helps in managing blood sugar levels, thereby delivering significant benefits for people struggling with diabetes. These gains significantly amplify when they're paired with strategic lifestyle modifications, particularly physical activities. Incorporating a regimen of consistent bodily exercises doesn't only bolster Ozempic's potency but also fosters a healthy lifestyle, which is essential for diabetes management. Activities such as brisk walking, cycling, swimming or any other form of moderate-intensity workout encourages weight loss. This reduction in body fat is key to reducing sugar levels and improving insulin sensitivity, thereby enhancing the medication's efficiency. Physical activity increases the body’s insulin sensitivity, which means that it can use insulin more effectively. When used optimally, Ozempic stimulates insulin release in a glucose-dependent manner, ultimately furnishing better control over blood sugar levels and facilitating successful diabetes management. Therefore, engaging in regular fitness routines can result in more significant effects of Ozempic in a shorter period, subsequently providing quicker relief from diabetes symptoms. Moreover, incorporating physical exercise into patient’s daily routines promotes a sense of wellbeing, reduces stress, and battles fatigue - common side effects associated with glucose management medications like Ozempic. Thus, not only does exercise have a profound effect on enhancing the potency of Ozempic, but it also cushions the system against possible side effects. In conclusion, the effective use of physical activity paired with Ozempic therapy offers a promising pathway in securing health benefits and achieving optimal effectiveness. This partnership between medicine and lifestyle adjustment is a clear testament to the philosophy of holistic treatment – tackling maladies not just via medications, but also through lifestyle modifications. The power of physical activity to boost Ozempic's effectiveness in managing diabetes and decreasing its onset period is irrefutable. The bond between the two showcases the need for a holistic approach, including medication and a healthy lifestyle, in the fight against diabetes.
Importance of compliance to medication schedule
The importance of complying with a medication schedule, particularly when taking Ozempic, cannot be overstated. Compliance to a medication schedule is vitally important for optimizing the effectiveness of Ozempic, along with lifestyle modifications. It is not just about popping a pill or injecting a solution at a given time, but about allowing the body to adjust and react optimally to the medication. When a medication is taken at the prescribed time, its effectiveness can be maximized and the benefits can be prolonged, because most drugs have a certain life cycle and work the best when they are taken regularly as per the schedule. Medication timetables are carefully designed by healthcare professionals based on the medicine's pharmacological properties such as its absorption rate, distribution path in the body, metabolization process, and excretion rate. Skipping or delaying a dose could disrupt this cycle, potentially reducing the drug's efficacy. Especially with a drug like Ozempic, used in the management of type 2 diabetes and weight loss, adherence to a medication schedule can significantly define the success of the treatment plan. In addition to this pharmacological perspective, every treatment recommendation, which includes medication instructions along with lifestyle modifications for optimal results, builds on a commitment to discipline and routine. Diet improvements, exercise commitments, along with medication, combine together to attain the desired health outcome. With Ozempic, the synergy between timely intake of medication and lifestyle changes such as diet and exercise can contribute to better glycemic control, weight loss, and improved long-term health. In conclusion, compliance to a medication schedule is not just a routine, it is a pivotal element of successful treatment. With Ozempic, consistently following a medication schedule, in combination with suitable lifestyle modifications, can enhance the effectiveness of treatment and result in substantial health improvements. Thus, making it critical to acknowledge and practice the importance of following a timely medication schedule to allow the body an optimal chance of leveraging the benefits of the drug, which in turn contributes to a healthier life.