How Do You Go To The Bathroom In An Iron Lung
 As one immerses in the 21st century's realm of advanced medical interventions, it can be intriguing to explore devices of yore that played pivotal roles in healthcare. One such marvel is the Iron Lung, a contraption whose name itself invokes awe and curiosity. This article aims to unravel the mysteries surrounding the Iron Lung, delving especially into a particular question that might seem unusual but holds significant relevance - How does one go to the bathroom while residing within this mechanical cocoon? We will first delve into understanding the Iron Lung, its historical role, structure, and functionality. Then we will scrutinize the logistics of basic necessities when inside this medical device, an aspect tha often takes a backseat amidst the life-saving discussions. In our final stride, we will shed light on an often overlooked but crucial factor - waste management inside this harbinger of hope. As we navigate through the intriguing pathways forged by this contraption, let's begin by 'understanding the Iron Lung.'
As one immerses in the 21st century's realm of advanced medical interventions, it can be intriguing to explore devices of yore that played pivotal roles in healthcare. One such marvel is the Iron Lung, a contraption whose name itself invokes awe and curiosity. This article aims to unravel the mysteries surrounding the Iron Lung, delving especially into a particular question that might seem unusual but holds significant relevance - How does one go to the bathroom while residing within this mechanical cocoon? We will first delve into understanding the Iron Lung, its historical role, structure, and functionality. Then we will scrutinize the logistics of basic necessities when inside this medical device, an aspect tha often takes a backseat amidst the life-saving discussions. In our final stride, we will shed light on an often overlooked but crucial factor - waste management inside this harbinger of hope. As we navigate through the intriguing pathways forged by this contraption, let's begin by 'understanding the Iron Lung.'Understanding the Iron Lung
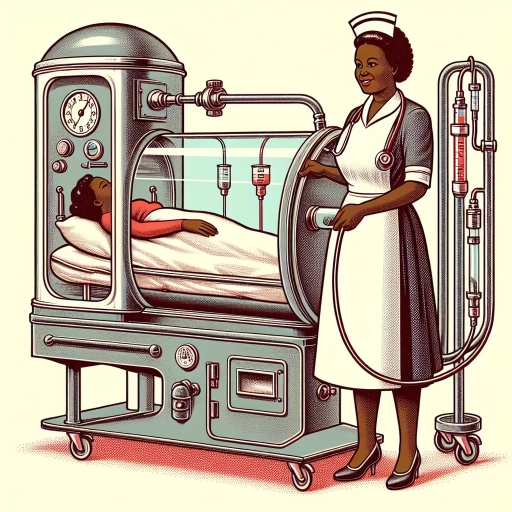
The iron lung, a remarkable medical device that once signified hope and survival for countless polio patients, remains a fascinating symbol of a bygone era in medical history. This article delves into the intricacies of understanding this notable contraption and presents three dimensions for better insights: The history and functionality of the Iron Lung, the challenges of living in an Iron Lung, and modern alternatives to the Iron Lung. By skimming the surface of these subjects, we aim to illuminate the story behind the Iron Lung. This colossal machine, imprinted in the annals of medical history, hid a complex interior where extraordinary things took place. It's intriguing to juxtapose this mechanical wonder with its daunting challenges, raising questions of human resilience and adaptability. Ultimately, we'll peer into the ever-evolving field of medical technology, analyzing the contemporary substitutes for the iron lung. As we transition into the first chapter, join us in exploring the origin and mechanics of this life-saving device, a compelling tale of innovation and necessity providing a foundational understanding of the Iron Lung.
The History and Functionality of the Iron Lung
In understanding the intricacies of the iron lung, one must first delve into its remarkable history and the function it serves. Born out of necessity during the Poliomyelitis outbreak in the early 20th century, the iron lung, also known as the Drinker Respirator, was a remarkable feat of medical engineering. This mechanical respirator was invented by Harvard medical researchers Philip Drinker and Louis Agassiz Shaw in 1927. The prime objective of the iron lung was to enable patients, whose respiratory muscles were incapacitated by polio, to breathe. It functioned by creating a vacuum that caused the patient's chest to expand, allowing air to flow into the lungs. When the vacuum was alleviated, the chest contracted and the air was expelled. This artificial mechanism of respiration enabled many paralytic polio victims to survive during the period when there was no effective vaccine for the virus. Despite its intimidating appearance — a large, airtight tube enveloping the patient’s body, with only the head protruding — the essence of the iron lung was its life-saving functionality. With the help of the iron lung, polio patients found a flicker of hope amidst the bleakness of their condition. This was before the invention of positive pressure ventilators, which powerfully forced the air into the patient's lungs and eventually led to the decline of the iron lung's use. While the iron lung may be an object of historical interest today, at its zenith, it was an indispensable tool in the fight against polio. It serves as a poignant reminder of the audacity of scientific innovation driven by utter necessity. Today, whilst largely replaced by more contemporary respirators, the iron lung remains etched in the collective medical memory as a symbol of human resilience in the face of desperate health crises. Understanding the iron lung's functionality isn't simply an exercise in medical history, but an insight into our perpetual struggle against infectious diseases.
Challenges of Living in an Iron Lung
Delving deeper into the functionings of the Iron Lung, it is necessary to understand the inherent challenges associated with living inside this contrivance. A primary issue lies in the pervasive sense of confinment. The patient, encased within the cylindrical iron chamber, with only their head exposed, are left at the mercy of their caretakers for the most basic necessities, including accessing the restroom. The question, "how do you go to the bathroom in an iron lung" surely provokes curiosity; the answer, however, embodies the essence of the struggle experienced by those living thus. The solution rests in undignified but necessary arrangements - urinals, bedpans, and incontinence pads. A catheter would be an expedient means to manage urinary issues, but it presents its own challenges within the confines of the machine. Handling bowel movements, on the other hand, requires a more clever workaround. Usually, a rectal tube attached to a colostomy bag is employed, thus permitting a certain degree of independence for the patient, and alleviating some of the burdens placed on the caretakers. Beyond the physical discomfort, the emotional toll can weigh heavily on the patient. Being dependent on others for even the most intimate actions, often leads to feelings of helplessness and depression. It also disruptively alters the relationship dynamics with the caretakers in ways that can be emotionally distressing for both parties. Furthermore, the inability to move around freely reinforces feelings of frustration and isolation. That said, those who have spent their lives in an iron lung have often demonstrated remarkable resilience and adaptability. While the extraordinary challenges are evident, many have forged meaningful lives despite the restrictions, suggesting that it is not the magnitude of the challenge that defines us, but our response to it. This seems particularly relevant when exploring the realities of life in an iron lung, illuminating the complexities of human determination in the face of adversity.
Modern Alternatives to the Iron Lung
Ever since the pivotal intervention of the iron lung, science has made significant strides in technological advancement, paving the way for several modern alternatives. Morphed from the concept of iron lung, these alternatives are designed with full consideration of patient comfort, lifestyle compatibility and enhanced functionality. One prominent alternative is the Positive Pressure Ventilator, commonly known by its brand name, BiPAP (Bilevel Positive Airway Pressure). Unlike the iron lung, which created a negative pressure environment for the patient to breathe, the BiPAP device employs positive pressure to push air into the patient’s lungs. Equipped with comfortably fitted nasal or facial masks, BiPAP machines are not only more compact and portable but also far less intimidating than the colossal iron lung. Modern medical scientists have also developed a similar but more refined technology named Continuous Positive Airway Pressure (CPAP). While BiPAP administers two levels of air pressure for inhaling and exhaling respectively, CPAP employs a single continuous pressure setting, making it an ideal solution for people with lesser severe breathing issues. Both these devices ensure uninterrupted sleep to the patients, contributing positively to their quality of life. Another breakthrough in the arsenal of iron lung alternatives is the Phrenic Nerve Pacemaker, which stimulates diaphragm movement by electronically triggering the phrenic nerve. This pacemaker, once implanted, aids the patient in their respiration process without any external apparatus. Notably, the late physicist Stephen Hawking was a user of this technology. In an era that values freedom of movement and lifestyle integration, yet another player has entered the field: the "wearable ventilator". A case in point is the Hayek RTX, which combines the principles of the old iron lung, but in a lightweight, wearable form. It optimizes the natural physiological breathing process without restricting mobility or compromising on social interactions. Though these modern alternatives don’t entirely dismiss the necessity or the significance of the iron lung, they do provide a more manageable and integrous way to respond to similar medical conditions. These technologies are a testament to the fact that evolution in medical science is perpetual and continues to enhance humanity's quality of life.
The Logistics of Basic Necessities in an Iron Lung
Living with an Iron Lung presents daunting challenges in managing basic needs. The simplistically mundane tasks become an ordeal when bound by the restrictions of this life-sustaining equipment. This article seeks to shed light on three critical aspects of daily life which turn into complex logistical exercises for patients in an Iron lung. From addressing the fundamental needs of eating and drinking, to maintaining personal hygiene, and accommodating the unavoidable realities of bodily functions - it unpacks the intricate routines that starkly contrast the ease of everyday life. Starting with accommodating for eating and drinking, a seemingly simple privilege of life suddenly amplified in complexity. The process requires innovative ideas, mechanical adjustments, and utmost precision to ensure the sustenance of vital nutrition and hydration. Let's delve into how patients have managed to surmount these hurdles, turning challenges into a testament of resilience and human adaptability.
Accommodating for Eating and Drinking
Accommodating for eating and drinking in an iron lung is an essential yet complex process, necessitating meticulous planning, a specialized diet, and the use of unique tools—all in an effort to maintain the patient's basic nutrition while limiting the risk of choking or other potential hazards. The patient's body is predominately enclosed within the metal machine, with the head sticking out, limiting physical motion and making standard eating and drinking methods practically impossible. Interaction with food and drink typically involved the use of extended, long-handled eating utensils and straws, which allowed caregivers to feed their patients. Unsurprisingly, the process proved more labor-intensive than usual and often required multiple members of family or nursing staff to be involved. What's more, the timing of meals was often finely tuned to match the machine's cycles, as the changing pressure within the lung could impede comfortable and safe swallowing. To navigate this, one popular method allowed patients to eat during the machine's 'exhalation' phase when external pressure is lowest, facilitating a less difficult swallowing process. The diet of an individual living within an iron lung needed to be carefully curated, considering both nutritional needs and ease of consumption. Soft, mashed foods that were easy to swallow and digest were a staple for many living in iron lungs. Additionally, liquid intake needed to be carefully regulated, balancing the need for hydration while keeping in mind the complexities and risks involved in drinking within the machine. Clinical technologies, nutritionists, and healthcare providers have since evolved a long way from the heavy reliance on iron lungs in the last century. However, examining these complexities offers a stark reminder of the extraordinary lengths that many men, women, and children once had to navigate to perform such a fundamental human act as eating and drinking. This discussion underscores the intricate logistics and countless considerations that were involved in providing basic necessities to those confined in an iron lung. From the intricate preparation process to the carefully planned timing, the mere act of eating or drinking became a challenging routine, testifying to the resilience and adaptability of both the patient and caregiver. It also showcases the immense advances in medical technology that have made managing conditions like polio safer and more efficient today. Reflecting on these aspects not only highlights the historical aspects of healthcare but sheds light on the silent struggles faced by those bound in iron lungs and the lengths taken by caregivers to afford their loved ones a semblance of normalcy in such challenging circumstances.
Dealing with Personal Hygiene
Maintaining personal hygiene is one of the most salient aspects to consider when coping with life in an iron lung. Ensuring cleanliness and sanitation is not only vital for the patient's physical health, but it also significantly uplifts their mental wellbeing and overall quality of life. As an individual encased within the iron lung apparatus primarily, it's paramount to exercise inventiveness in devising hygiene routines that adhere to their unique circumstances without jeopardizing their health. A meticulous plan for daily routine tasks, like washing, grooming and dental hygiene, is a cornerstone to achieving this. Firstly, sponge baths are typically the primary means of cleansing in these situations. The delicate procedure requires a trained caregiver to carefully wash the exposed parts of the patient's body - the head, neck, and parts of the limbs, dependent on the specifics of the patient's condition. It becomes essential to employ gentle, hypoallergenic cleansing agents that reduce the risk of skin irritation, especially considering the reduced mobility of the patient. Secondly, grooming tasks such as combing hair, trimming nails, and even applying makeup where desired, are integral to making the patient feel cared for and maintaining their sense of human dignity. Adapted tools, steady hands, and a patient approach are key in undertaking these tasks smoothly. Additionally, oral hygiene becomes even more critical for the individual, not only in preventing dental issues but also in averting any infections that could exacerbate respiratory problems. Extra-soft toothbrushes, antimicrobial mouthwashes, and dental wipes help maintain oral cleanliness and promote overall health. The above-mentioned practices, while practical, also hold a metaphorical significance in the arduous journey of an iron lung resident. They endow the individual with a semblance of independence and personal agency - crucial factors in nurturing mental resilience against their physically challenging everyday experience. Above all else, ensuring patient comfort during these routines is cardinal; not merely as a matter of sensitivity, but also because any discomfort could lead to jeopardizing their respiratory assistance. Thus, the logistics of delivering personal hygiene care in an iron lung become a delicate dance between maintaining physical cleanliness and upholding the psychological aspects of well-being intertwined with the act of personal care. In a sense, it's not just about the act of bathing or brushing teeth, but about preserving the patient's dignity and resilience under challenging conditions.
Addressing the Bodily Functions
Living in a confined contraption might seem unthinkable in terms of addressing basic bodily functions, but contrary to what one might imagine, addressing the logistical considerations of these functions in an iron lung is an astounding feat of engineering and medical ingenuity. Think of it as a self-contained, intricate ecosystem that's designed to maintain a delicate balance. Firstly, consider urinary and bowel movements, key bodily functions that undergo significant readjustment when living within the confines of an iron lung. Physicians and engineers tasked with the responsibility of providing comfortable living conditions for the patients, focused on creating a system that quietly and efficiently manages these functions. Bedpans and urinals are traditionally used, diligently maintained by healthcare personnel to ensure utmost hygiene. Specialized designs of these utensils with elongated handles and spill-proof structures have been devised for convenience and minimum interference. Secondly, the aspect of perspiration management in an iron lung is worth noting. These machines are traditionally housed in cool, well-ventilated rooms to thwart overheating and excessive sweating. The interiors are fitted with absorbent and easy-to-change linen to mop up sweat, and the patient's skin is regularly cleaned to prevent rashes or sores. Additionally, menstrual management for female patients is another factor taken into consideration. Using specially designed sanitary products which can be easily replaced and disposed of, the process is made a lot less daunting, whilst maintaining the dignity and comfort of the patient. This paragraph discusses the process of practical and effective strategies to enable basic bodily functions in an iron lung, yet, it's important to underscore that living in such a contraption doesn't come without severe adaptations and new learning curves. Each patient has to learn to adjust and communicate their needs effectively, while healthcare providers work tirelessly to maintain a clean, healthy, and dignified living environment within the iron lung. This segment signifies the resilience of the human spirit and the remarkable advances in medical and healthcare engineering that made such a life possible.
How Waste Management Works in an Iron Lung
Waste management in an Iron Lung, an essential yet often overlooked aspect, plays a critical role in enhancing the well-being and comfort of the patient. It primarily involves three crucial facets: the use of catheters and bedpans, the integral role of caregivers, and the ongoing advancements in waste management strategies. First, we delve into the world of catheters and bedpans, indispensable tools that aid in the disposal of human waste while maintaining a hygienic environment. They exemplify ingenuity in simplicity, exhibiting how even the most straightforward solutions can exceptionally address complex challenges. As we move further, we shed light on the paramount role that caregivers undertake in managing the waste. From ensuring proper utilization of equipment to taking proactive steps for avoiding potential risks associated with incorrect disposal, they serve as the unsung heroes in patient care. Lastly, we'll explore the innovations and improvements in this domain, spotlighting the modern progresses that aim to refine the process and promise a better tomorrow for Iron Lung users. Now, let's delve into the first facet and decode the science behind the use of catheters and bedpans.
The use of Catheters and Bedpans
In understanding the utilization of waste management in an iron lung, it's essential to bring into focus the significant role played by devices such as catheters and bedpans. As part of a comprehensive waste management system in an otherwise confined bodily scenario, these tools make seemingly impossible tasks executable. A catheter, traditionally, is a thin tube made from medical grade materials that serve a broad range of functions. In the scenario of an iron lung, a catheter's primary function is to assist with voiding urine directly from the bladder. The bladder, although inhibited by the confinement of the iron lung, still functions normally, producing urine, and thus necessitates regular emptying. To make this feasible, a Foley catheter, a distinct kind designed for prolonged usage, is commonly used. This catheter has a small, inflated balloon on one end that keeps the system in place within the bladder, allowing urine to continuously flow into a specially designed bag. This kind of automated, continuous management works marvellously in the bodily constrictions set by an iron lung. Simultaneously, solid waste management can be more complex but is nevertheless crucial. Here's where bedpans come into action providing a synchronized solution to an otherwise challenging problem. The challenge in using the bedpan while confined to an iron lung rests in the discomfort and potential hygiene issues. However, with meticulous maintenance and proper care from trained health personnel, this issue can be mitigated, maintaining the dignity and well-being of the patient. The intersection of catheters and bedpans in the waste management system of an iron lung plays a pivotal role in normalizing the experience for the patient. The brilliance of these methods lies in their functionality and the relief they bring to patients, ensuring them a dignified experience during this trying ordeal of confinement in an iron lung. The provision of waste clearance that synced with the natural bodily functions significantly enhances the operation and patients' overall experience within the device, resulting in these instruments being hailed as unsung heroes in the tale of the iron lung.
The Role of Caregivers in Waste Management
The Role of Caregivers in Waste Management is a pivotal and often underestimated part of the daily routine in the care of patients confined in an iron lung. The iron lung, a negative pressure ventilator primarily utilized during the polio epidemics of the 20th century, facilitates breathing for patients incapable to do so due to muscle impairment. Physical confines imposed by this life-saving machine necessitate an elaborate system of waste management, with caregivers playing a crucial role. As the patient's main physical conduit to the outside world, caregivers take on numerous responsibilities in terms of hygiene and waste disposal. Their role in waste management begins with strategizing an effective waste disposal plan tailored to the specific needs of the patient and the type of iron lung in use. The challenge lies in ensuring minimal disruption to both the patient's comfort and the machine's workings during the disposal processes. Assuredly, caregivers use specialized equipment for urine and fecal disposal. Excretory waste is typically managed through intermittent catheterization or the use of adult diapers, depending on the patient's specific conditions. The waste materials are then carefully collected and stored before they are safely disposed of following local medical waste regulations. This process requires diligent sanitation to prevent infections, which could lead to complications in patients with already compromised respiratory systems. Apart from bodily wastes, caregivers must also manage other forms of waste, like used medical supplies and disposable items. For instance, the disposable circuits of the iron lung need a meticulous replacement and disposal routine. Caregivers must be highly organized, maintaining separate waste bins for different kinds and meticulously following scheduled waste collection and disposal timings. Caregivers also have to keep track of the products used in patient care, such as cleaning agents and laundry detergents. They should ideally opt for eco-friendly options to minimize environmental impact, highlighting their responsibility extends beyond the patient to also encompass environmental guardianship. In summary, the caregiver’s role in waste management goes hand in hand with their function as an essential link between the patient and the world beyond the iron lung. They coordinate multiple delicate tasks, from managing bodily waste with minimal intrusion to regulating disposable medical supplies, all while adhering to stringent sanitation standards and environmental considerations. Therefore, the success of waste management within the exceptional environment of the iron lung greatly hinges on the detailed work of these unsung heroes.
Current Innovations and Improvements in Waste Management for Iron Lung Users
Emerging technologies and breakthroughs in the field of waste management for Iron Lung users have led to significant refinements and improvements in the method. In-depth awareness of this arcane subject is crucial as we continue to push the boundaries of patient care and seek opportunities to enhance the quality of life for those bound to iron lungs. Regulating waste management in an iron lung typically employs a catheter to deal with urinary waste and a bedpan for solid waste. These components, however, fall short of being comfortably and seamlessly manageable, indicating the need for advancements in this crucial aspect of healthcare. One of the most significant advancements in waste management for iron lung users is the development of 'Smart Catheters.' These are intelligent medical devices that can monitor infection indicators in urine, alerting healthcare providers to signs of imminent infection. This real-time data collection and analysis create a safe, efficient, and proactive waste management system, significantly reducing the risk of urinary tract infections. Additionally, biodegradable bedpans have seen significant improvements, providing a more environmentally-friendly and sanitary solution. Made of recycled pulp or sugarcane bagasse, these bedpans are sturdy, comfortable, and can be conveniently decomposed after single use, eliminating the need for manual cleaning and the risk of cross-contamination. Another noteworthy innovation is the evolving design of the iron lung itself. Modern medical equipment companies are now integrating a waste management system directly into iron lung designs, removing the need for additional, sometimes cumbersome, devices. These integrated systems can better accommodate the bowel and urinary needs of the patient in a more streamlined and discreet manner. Intriguing solutions are also surfacing from the field of robotics, employing robotic care systems attached to the iron lung which handle waste collection, hygiene assistance, and can even facilitate patient debilitation. These emerging innovations are paving the way for more efficient, less invasive, and overall improved waste management solutions for iron lung users. With technological advancements, the prospect of elevating the living standards of iron lung patients becomes a more tangible goal, demonstrating the profound potential of innovation in this medical frontier.