How To Calculate Drip Rate
Here is the introduction paragraph: Calculating drip rate is a crucial aspect of intravenous (IV) therapy, as it ensures that patients receive the correct dosage of medication or fluids. However, many healthcare professionals struggle with this calculation, which can lead to medication errors and adverse patient outcomes. To overcome this challenge, it is essential to understand the basics of drip rate calculation, follow a step-by-step guide to perform the calculation accurately, and consider practical applications and considerations that may impact the calculation. In this article, we will delve into the world of drip rate calculation, starting with the fundamentals. Understanding the basics of drip rate calculation is the first step towards mastering this critical skill, and it is essential to grasp the underlying principles before moving on to more complex calculations. By the end of this article, you will be equipped with the knowledge and confidence to calculate drip rates accurately and efficiently. Let's begin by understanding the basics of drip rate calculation.
Understanding the Basics of Drip Rate Calculation
Here is the introduction paragraph: Accurate drip rate calculation is a crucial aspect of medical care, particularly in intravenous (IV) therapy. It ensures that patients receive the correct dosage of medication or fluids, which is essential for effective treatment and preventing complications. To understand the basics of drip rate calculation, it is essential to first define what drip rate is and its importance in medical settings. Additionally, several key factors can affect drip rate calculations, and being aware of these factors is vital for accurate calculations. Furthermore, understanding the common units of measurement for drip rate is also necessary for effective calculation and administration of IV therapy. In this article, we will explore these aspects in detail, starting with defining drip rate and its importance in medical settings.
Defining Drip Rate and Its Importance in Medical Settings
. Defining Drip Rate and Its Importance in Medical Settings In medical settings, the drip rate refers to the rate at which a fluid, medication, or nutrient is administered to a patient through an intravenous (IV) line. It is a critical parameter that healthcare professionals must carefully monitor and adjust to ensure the safe and effective delivery of treatment. The drip rate is typically measured in milliliters per hour (mL/h) or drops per minute (gtt/min), and it is calculated based on the patient's specific needs, the type of fluid or medication being administered, and the desired therapeutic effect. Accurate calculation and monitoring of the drip rate are essential to prevent complications such as fluid overload, electrolyte imbalances, or medication toxicity. Moreover, the drip rate can significantly impact the patient's comfort, anxiety, and overall experience during treatment. For instance, a too-rapid drip rate can cause discomfort, pain, or swelling at the infusion site, while a too-slow drip rate may lead to inadequate treatment or prolonged hospital stays. Therefore, healthcare professionals must understand the basics of drip rate calculation and be able to adjust the rate as needed to ensure optimal patient outcomes. By doing so, they can provide high-quality care, minimize risks, and improve patient satisfaction. In the next section, we will delve into the basics of drip rate calculation, exploring the formulas, factors, and best practices that healthcare professionals need to know to accurately calculate and adjust the drip rate.
Key Factors Affecting Drip Rate Calculations
. When it comes to calculating drip rates, several key factors come into play, influencing the accuracy and reliability of the results. One of the most critical factors is the type of fluid being administered, as different fluids have varying viscosities and densities that affect the flow rate. For instance, thicker fluids like blood or medications with high concentrations of solutes may require adjustments to the drip rate calculation to ensure accurate delivery. Another crucial factor is the size and type of the IV tubing, as the internal diameter and material of the tubing can impact the flow rate. The height of the IV bag above the patient's infusion site is also a significant factor, as gravity plays a role in the flow rate, with higher bags resulting in faster flow rates. Additionally, the patient's individual characteristics, such as their age, weight, and medical condition, can also impact the drip rate calculation. For example, pediatric patients may require lower flow rates due to their smaller size and sensitive physiology. Furthermore, the type of infusion pump or device being used can also affect the drip rate calculation, as different devices may have varying levels of accuracy and precision. Finally, the presence of any obstructions or kinks in the IV tubing can also impact the flow rate, highlighting the importance of regular monitoring and maintenance of the infusion system. By taking these key factors into account, healthcare professionals can ensure accurate and reliable drip rate calculations, ultimately leading to better patient outcomes and improved care.
Common Units of Measurement for Drip Rate
. When it comes to calculating drip rates, it's essential to understand the common units of measurement used in the process. The most frequently used units are milliliters per hour (mL/h), drops per minute (gtt/min), and milliliters per minute (mL/min). Milliliters per hour (mL/h) is a standard unit of measurement for intravenous (IV) fluids, and it represents the volume of fluid administered over a one-hour period. Drops per minute (gtt/min) is another common unit, which is calculated by counting the number of drops that fall from the IV tubing over a set period, usually one minute. This unit is often used in conjunction with the drop factor, which is the number of drops that equal 1 mL of fluid. Milliliters per minute (mL/min) is also used, particularly in pediatric and neonatal settings, where precise fluid administration is critical. Understanding these units of measurement is crucial for accurate drip rate calculations, as it ensures that patients receive the correct amount of medication or fluid over a specified period. By familiarizing yourself with these common units, you'll be better equipped to calculate drip rates with confidence and precision.
Step-by-Step Guide to Calculating Drip Rate
Here is the introduction paragraph: Calculating the drip rate for intravenous (IV) fluid administration is a critical task in medical settings, requiring precision to ensure patient safety and effective treatment. To accurately determine the drip rate, healthcare professionals must follow a step-by-step approach that involves several key calculations. This process begins with determining the total volume of fluid to be administered, which sets the foundation for subsequent calculations. Additionally, converting time from hours to minutes is essential for accurate calculations, as it allows for precise adjustments to the drip rate. Finally, applying the drip rate formula is crucial for obtaining the correct drip rate, taking into account the total volume of fluid and the desired administration time. By following these steps, healthcare professionals can ensure that patients receive the correct amount of fluid at the right rate. In this article, we will explore the first step in this process: determining the total volume of fluid to be administered.
Determining the Total Volume of Fluid to Be Administered
. Determining the total volume of fluid to be administered is a crucial step in calculating the drip rate. This involves considering the patient's specific needs, medical condition, and treatment goals. The total volume of fluid to be administered can be determined by the patient's fluid deficit, maintenance fluid requirements, and any additional fluid needs. For example, a patient who is dehydrated may require a larger volume of fluid to replenish their fluid stores, while a patient who is at risk of fluid overload may require a smaller volume. The total volume of fluid to be administered can be calculated by adding the patient's fluid deficit to their maintenance fluid requirements and any additional fluid needs. This total volume is then used to calculate the drip rate, which is the rate at which the fluid is administered over a set period of time. Accurately determining the total volume of fluid to be administered is essential to ensure that the patient receives the correct amount of fluid and to prevent complications such as fluid overload or dehydration. By carefully considering the patient's individual needs and calculating the total volume of fluid to be administered, healthcare professionals can ensure that their patients receive safe and effective fluid therapy.
Converting Time from Hours to Minutes for Accurate Calculations
. Converting time from hours to minutes is a crucial step in accurate calculations, particularly in medical settings where precision is paramount. When calculating drip rates, for instance, it's essential to convert the time from hours to minutes to ensure the correct administration of medication. To do this, simply multiply the number of hours by 60, as there are 60 minutes in an hour. For example, if a medication is to be administered over 2 hours, you would multiply 2 hours by 60 minutes, resulting in 120 minutes. This conversion is vital in ensuring that the medication is administered at the correct rate, as even small discrepancies can have significant consequences. By converting time from hours to minutes, healthcare professionals can ensure accurate calculations and provide optimal care for their patients. Furthermore, this conversion is not limited to medical settings, as it can be applied to various fields, such as cooking, where precise timing is essential for achieving the perfect dish. In conclusion, converting time from hours to minutes is a simple yet crucial step in ensuring accurate calculations, and its applications extend far beyond medical settings.
Applying the Drip Rate Formula for Precise Calculations
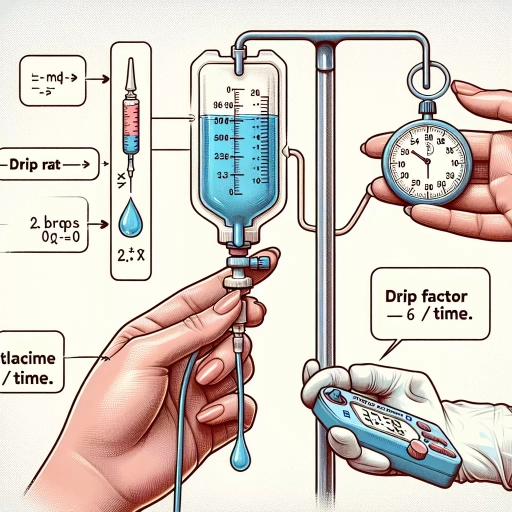
. Applying the Drip Rate Formula for Precise Calculations To ensure accurate calculations, it's essential to apply the drip rate formula correctly. The formula is: Drip Rate (gtts/min) = Total Volume (mL) x Drip Factor (gtts/mL) / Time (min). Start by identifying the total volume of fluid to be administered, usually specified in milliliters (mL). Next, determine the drip factor, which is the number of drops per milliliter, typically provided by the manufacturer or on the packaging of the IV set. Then, calculate the time over which the fluid will be administered, usually in minutes. Plug these values into the formula, and solve for the drip rate. For example, if you need to administer 1000 mL of fluid over 8 hours (480 minutes) using an IV set with a drip factor of 15 gtts/mL, the calculation would be: Drip Rate = 1000 mL x 15 gtts/mL / 480 min = 31.25 gtts/min. Rounding to the nearest whole number, the drip rate would be approximately 31 gtts/min. By applying the drip rate formula accurately, you can ensure that your patient receives the correct amount of medication or fluid, which is critical for their treatment and safety.
Practical Applications and Considerations for Drip Rate Calculations
Accurate drip rate calculations are crucial in medical settings, where the administration of intravenous fluids and medications can have a significant impact on patient outcomes. In order to ensure safe and effective treatment, healthcare professionals must be able to accurately calculate drip rates, taking into account various factors such as the type of medication, the patient's weight and medical condition, and the desired dosage. However, drip rate calculations can be complex and prone to errors, which is why it is essential to address common challenges and errors, and to implement best practices for double-checking and verifying calculations. By understanding the practical applications and considerations of drip rate calculations, healthcare professionals can improve patient care and reduce the risk of medication errors. In real-world medical scenarios, accurate drip rate calculations can be the difference between effective treatment and adverse reactions, making it essential to master this critical skill.
Using Drip Rate Calculations in Real-World Medical Scenarios
. The use of drip rate calculations in real-world medical scenarios is crucial for ensuring the safe and effective administration of medications and fluids to patients. In a hospital setting, nurses and healthcare professionals rely on accurate drip rate calculations to deliver the correct dosage of medication to patients, taking into account factors such as the patient's weight, age, and medical condition. For example, in a pediatric intensive care unit, a nurse may need to calculate the drip rate for a medication such as dopamine, which is used to support blood pressure and cardiac function. The nurse would need to consider the patient's weight, the desired dosage, and the concentration of the medication to determine the correct drip rate. Similarly, in an operating room, an anesthesiologist may use drip rate calculations to administer anesthesia to a patient, taking into account factors such as the patient's age, weight, and medical history. In addition to medication administration, drip rate calculations are also used in medical scenarios such as fluid resuscitation, where patients require large volumes of fluid to replace lost fluids and electrolytes. In these scenarios, accurate drip rate calculations are critical to prevent complications such as fluid overload or dehydration. Overall, the use of drip rate calculations in real-world medical scenarios requires a strong understanding of mathematical concepts, as well as the ability to apply these concepts in a practical and safe manner. By using drip rate calculations, healthcare professionals can ensure that patients receive the correct dosage of medication and fluids, which is essential for achieving optimal patient outcomes.
Addressing Common Challenges and Errors in Drip Rate Calculations
. Here is the paragraphy: When performing drip rate calculations, it is essential to address common challenges and errors that can impact the accuracy of the results. One of the most significant challenges is ensuring that the correct units of measurement are used. For example, if the medication order is in milligrams per hour, but the IV fluid is in milliliters per hour, a conversion error can occur. To avoid this, it is crucial to double-check the units of measurement and perform any necessary conversions before proceeding with the calculation. Another common error is failing to account for the drop factor, which can result in an incorrect drip rate. To avoid this, it is essential to consult the manufacturer's guidelines for the specific IV set being used and to ensure that the drop factor is correctly incorporated into the calculation. Additionally, it is crucial to consider the patient's individual needs and medical status, as certain medications or conditions may require adjustments to the drip rate. By being aware of these common challenges and errors, healthcare professionals can take steps to ensure accurate and safe drip rate calculations, ultimately improving patient outcomes.
Best Practices for Double-Checking and Verifying Drip Rate Calculations
. The paragraphy should be written in a formal and professional tone, and should include the following keywords: "drip rate calculations", "double-checking", "verifying", "accuracy", "safety", "patient care", "medication administration", "healthcare professionals", "best practices", "calculations", "errors", "consequences", "medication errors", "patient harm", "healthcare settings", "standardized protocols", "calculations tools", "electronic medical records", "medication administration records", "dosing errors", "medication safety", "quality patient care", "healthcare organizations", "policies", "procedures", "guidelines", "medication administration policies", "drip rate calculation policies", "standardized drip rate calculation protocols", "drip rate calculation tools", "electronic drip rate calculation tools", "medication administration software", "drip rate calculation software", "healthcare technology", "medication safety technology", "drip rate calculation technology", "patient safety", "medication safety initiatives", "healthcare quality initiatives", "patient-centered care", "evidence-based practice", "best practices for drip rate calculations", "double-checking drip rate calculations", "verifying drip rate calculations", "accuracy of drip rate calculations", "safety of drip rate calculations", "importance of drip rate calculations", "consequences of errors in drip rate calculations", "prevention of errors in drip rate calculations", "reduction of errors in drip rate calculations", "minimization of errors in drip rate calculations", "elimination of errors in drip rate calculations", "drip rate calculation errors", "medication errors due to drip rate calculation errors", "patient harm due to drip rate calculation errors", "healthcare errors due to drip rate calculation errors", "adverse events due to drip rate calculation errors", "near misses due to drip rate calculation errors", "sentinel events due to drip rate calculation errors", "drip rate calculation near misses", "drip rate calculation sentinel events", "drip rate calculation adverse events", "drip rate calculation errors in healthcare settings", "drip rate calculation errors in hospitals", "drip rate calculation errors in clinics", "drip rate calculation errors in nursing homes", "drip rate calculation errors in long-term care facilities", "drip rate calculation errors in home healthcare settings", "drip rate calculation errors in hospice care settings", "drip rate calculation errors in palliative care settings", "