How To Read Hospital Icu Monitor
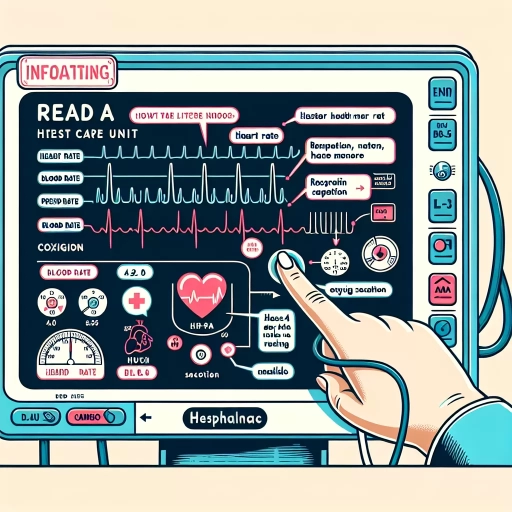
Here is the introduction paragraph: In a hospital's Intensive Care Unit (ICU), patients' conditions can change rapidly, and timely interventions are crucial. ICU monitors play a vital role in tracking patients' vital signs and alerting healthcare professionals to potential issues. To effectively care for critically ill patients, it is essential to understand how to read ICU monitors. This article will guide you through the process, starting with the basics of ICU monitors, including the various components and their functions. We will then delve into interpreting vital signs, such as heart rate, blood pressure, and oxygen saturation, and discuss how to identify trends and abnormalities. Finally, we will explore advanced features and alarms on ICU monitors, including how to customize settings and respond to alerts. By mastering these skills, healthcare professionals can provide better care and improve patient outcomes. Let's begin by understanding the basics of ICU monitors.
Understanding the Basics of ICU Monitors
In the high-stakes environment of an intensive care unit (ICU), having the right equipment is crucial for patient care. ICU monitors are a vital part of this equipment, providing healthcare professionals with real-time data on a patient's vital signs and other critical health metrics. But what exactly is an ICU monitor, and what makes it different from other medical monitors? To understand the basics of ICU monitors, it's essential to break down their components and purpose. This includes understanding the common components that make up an ICU monitor, how these monitors differ from other medical monitors, and what an ICU monitor is and its purpose. By exploring these aspects, healthcare professionals can better utilize ICU monitors to provide optimal patient care. So, let's start by examining what an ICU monitor is and its purpose.
What is an ICU Monitor and Its Purpose
An ICU monitor, also known as a critical care monitor, is a medical device used to continuously track and display a patient's vital signs and other physiological parameters in real-time. The primary purpose of an ICU monitor is to provide healthcare professionals with accurate and timely information about a patient's condition, enabling them to make informed decisions about their care. ICU monitors are typically used in intensive care units (ICUs), emergency departments, and operating rooms, where patients require close monitoring due to life-threatening illnesses or injuries. These monitors display a range of data, including electrocardiogram (ECG) readings, blood pressure, oxygen saturation, respiratory rate, and temperature, among others. By analyzing this data, healthcare professionals can quickly identify any changes or abnormalities in a patient's condition, allowing them to respond promptly and effectively to prevent complications or deterioration. Overall, the purpose of an ICU monitor is to enhance patient safety, improve outcomes, and facilitate high-quality care in critical care settings.
Common Components of an ICU Monitor
The ICU monitor is a complex device that displays a wide range of vital signs and other important data to help healthcare professionals make informed decisions about patient care. Some common components of an ICU monitor include the electrocardiogram (ECG) display, which shows the patient's heart rhythm and rate; the blood pressure display, which shows the patient's systolic and diastolic blood pressure; and the oxygen saturation (SpO2) display, which shows the percentage of oxygen in the patient's blood. Other common components include the respiratory rate display, which shows the number of breaths the patient takes per minute; the tidal volume display, which shows the volume of air inhaled and exhaled by the patient; and the end-tidal CO2 (ETCO2) display, which shows the level of carbon dioxide in the patient's exhaled breath. Additionally, many ICU monitors also display other important data, such as the patient's temperature, cardiac output, and blood glucose levels. By displaying all of this information in one place, ICU monitors provide healthcare professionals with a comprehensive view of the patient's condition, allowing them to quickly identify any changes or abnormalities and take prompt action to address them.
How ICU Monitors Differ from Other Medical Monitors
ICU monitors differ from other medical monitors in several key ways. Firstly, ICU monitors are designed to provide a comprehensive view of a patient's critical vital signs and physiological parameters in real-time, allowing healthcare professionals to quickly identify any changes or abnormalities. In contrast, other medical monitors may only track a limited set of vital signs, such as heart rate and blood pressure, and may not provide the same level of detail or frequency of updates. Additionally, ICU monitors often include advanced features such as arrhythmia detection, cardiac output monitoring, and invasive blood pressure monitoring, which are not typically found on other medical monitors. Furthermore, ICU monitors are designed to be highly customizable, allowing healthcare professionals to tailor the display and alarms to meet the specific needs of each patient. This level of customization is not typically available on other medical monitors, which may have more limited configuration options. Overall, the advanced features, customization options, and real-time data provided by ICU monitors make them an essential tool for healthcare professionals working in intensive care units.
Interpreting Vital Signs on ICU Monitors
Interpreting vital signs on ICU monitors is a crucial skill for healthcare professionals to master, as it enables them to quickly identify potential issues and make informed decisions about patient care. Vital signs, including heart rate and rhythm, blood pressure, and oxygen saturation, provide valuable insights into a patient's overall health and well-being. By understanding how to interpret these signs, healthcare professionals can detect subtle changes in a patient's condition and respond promptly to prevent complications. In this article, we will delve into the world of ICU monitoring, exploring the intricacies of heart rate and rhythm displays, blood pressure and mean arterial pressure readings, and oxygen saturation and respiratory rate displays. By the end of this article, healthcare professionals will be equipped with the knowledge and skills necessary to accurately interpret vital signs and provide high-quality patient care. Let's start by examining the complexities of heart rate and rhythm displays.
Understanding Heart Rate and Rhythm Displays
Understanding Heart Rate and Rhythm Displays is crucial when interpreting vital signs on ICU monitors. The heart rate display shows the number of beats per minute (bpm), which is typically measured in real-time using electrocardiogram (ECG) leads. A normal heart rate for adults ranges from 60 to 100 bpm, while for children and infants, it can be higher. The rhythm display, on the other hand, shows the pattern of the heartbeat, which can be regular or irregular. A regular rhythm is characterized by a consistent pattern of P-waves, QRS complexes, and T-waves, while an irregular rhythm can indicate arrhythmias or other cardiac issues. ICU monitors often display the heart rate and rhythm in numerical and graphical formats, allowing healthcare professionals to quickly identify any abnormalities. For example, a heart rate of 120 bpm with a regular rhythm may indicate tachycardia, while a heart rate of 40 bpm with an irregular rhythm may indicate bradycardia or a more serious cardiac condition. By understanding heart rate and rhythm displays, healthcare professionals can quickly identify potential issues and take prompt action to ensure the best possible patient outcomes.
Interpreting Blood Pressure and Mean Arterial Pressure Readings
Interpreting Blood Pressure and Mean Arterial Pressure Readings Blood pressure (BP) and mean arterial pressure (MAP) are two crucial vital signs that provide valuable information about a patient's cardiovascular status. Blood pressure is the force exerted by the blood against the walls of the arteries, while mean arterial pressure is the average pressure in the arteries during one cardiac cycle. To interpret BP and MAP readings, it's essential to understand the normal ranges and the implications of abnormal values. A normal blood pressure reading is typically considered to be between 90/60 mmHg and 120/80 mmHg, with the top number representing systolic pressure (the pressure when the heart beats) and the bottom number representing diastolic pressure (the pressure when the heart rests). Mean arterial pressure, on the other hand, is calculated by adding the systolic and diastolic pressures and dividing by 3, and a normal MAP reading is typically between 70-110 mmHg. Abnormal BP and MAP readings can indicate a range of conditions, including hypertension, hypotension, and cardiac dysfunction. For example, a patient with a BP reading of 180/100 mmHg may be experiencing hypertension, while a patient with a MAP reading of 40 mmHg may be at risk of organ perfusion. By closely monitoring BP and MAP readings, healthcare providers can quickly identify changes in a patient's condition and make informed decisions about their care. In the ICU setting, BP and MAP readings are often displayed on a monitor, allowing healthcare providers to track changes in real-time and respond promptly to any abnormalities. By understanding the significance of BP and MAP readings, healthcare providers can provide more effective care and improve patient outcomes.
Understanding Oxygen Saturation and Respiratory Rate Displays
Understanding oxygen saturation and respiratory rate displays is crucial for healthcare professionals to assess a patient's respiratory status and make informed decisions. Oxygen saturation, measured as SpO2, represents the percentage of hemoglobin in the blood that is saturated with oxygen. A normal SpO2 range is typically between 95% and 100%. The respiratory rate display shows the number of breaths a patient takes per minute, with a normal range of 12-20 breaths per minute for adults. When interpreting these displays, it's essential to consider the patient's underlying medical condition, age, and other vital signs. For example, a patient with chronic obstructive pulmonary disease (COPD) may have a lower SpO2 due to their condition, while a patient with pneumonia may have an increased respiratory rate. By monitoring these displays, healthcare professionals can quickly identify any changes in a patient's respiratory status and take prompt action to address any issues. Additionally, understanding oxygen saturation and respiratory rate displays can help healthcare professionals to titrate oxygen therapy and adjust ventilator settings to optimize patient care. By combining this information with other vital signs, such as heart rate and blood pressure, healthcare professionals can gain a comprehensive understanding of a patient's overall health status and make informed decisions to improve patient outcomes.
Advanced Features and Alarms on ICU Monitors
ICU monitors are equipped with advanced features and alarms that enable healthcare professionals to closely monitor patients' vital signs and respond promptly to any changes in their condition. These features and alarms are designed to provide critical information about a patient's cardiovascular, respiratory, and neurological status, among other parameters. In this article, we will delve into the advanced features and alarms on ICU monitors, exploring how they support patient care. We will examine the importance of understanding cardiac output and stroke volume displays, as well as interpreting invasive blood pressure and central venous pressure readings. Additionally, we will discuss the alarm systems and prioritization on ICU monitors, highlighting their role in ensuring timely interventions. By understanding these advanced features and alarms, healthcare professionals can optimize patient care and improve outcomes. Let's start by exploring the significance of cardiac output and stroke volume displays in patient monitoring.
Understanding Cardiac Output and Stroke Volume Displays
Understanding Cardiac Output and Stroke Volume Displays is crucial for healthcare professionals working in the ICU. Cardiac output (CO) is the volume of blood the heart pumps per minute, while stroke volume (SV) is the amount of blood pumped by the left ventricle of the heart in one contraction. ICU monitors display these values in real-time, allowing clinicians to assess cardiac function and make informed decisions. Cardiac output is typically measured in liters per minute (L/min), while stroke volume is measured in milliliters (mL). A normal cardiac output ranges from 4-8 L/min, while a normal stroke volume ranges from 60-100 mL. Abnormal values may indicate cardiac dysfunction, hypovolemia, or other underlying conditions. By monitoring cardiac output and stroke volume, clinicians can quickly identify changes in a patient's condition and adjust treatment accordingly. For example, a decrease in cardiac output may indicate the need for fluid resuscitation or inotropic support. In contrast, an increase in cardiac output may suggest the need to reduce fluid administration or adjust vasoactive medications. By understanding the displays and trends of cardiac output and stroke volume, healthcare professionals can provide more effective and targeted care to critically ill patients.
Interpreting Invasive Blood Pressure and Central Venous Pressure Readings
Invasive blood pressure (IBP) and central venous pressure (CVP) readings are crucial parameters monitored in the ICU to assess a patient's cardiovascular and hemodynamic status. IBP readings are obtained through an arterial catheter inserted into a major artery, typically the radial or femoral artery, and provide a direct measurement of blood pressure. CVP readings, on the other hand, are obtained through a central venous catheter inserted into a major vein, typically the internal jugular or subclavian vein, and provide an indirect measurement of the pressure in the right atrium. To interpret these readings, it's essential to understand the normal ranges and the clinical context in which they are being monitored. Normal IBP readings typically range from 90-120 mmHg systolic and 60-80 mmHg diastolic, while normal CVP readings typically range from 2-8 mmHg. Elevated IBP readings may indicate hypertension, while decreased readings may indicate hypotension. Elevated CVP readings may indicate fluid overload, cardiac dysfunction, or pulmonary hypertension, while decreased readings may indicate hypovolemia or cardiac tamponade. It's also important to consider the waveform and trend of the readings, as well as the patient's overall clinical picture, to make accurate interpretations and inform treatment decisions. For example, a patient with a high CVP reading and a flat waveform may indicate cardiac dysfunction, while a patient with a low CVP reading and a steep waveform may indicate hypovolemia. By carefully interpreting IBP and CVP readings, healthcare providers can gain valuable insights into a patient's cardiovascular and hemodynamic status, and make informed decisions to optimize their care.
Understanding Alarm Systems and Prioritization on ICU Monitors
Understanding alarm systems and prioritization on ICU monitors is crucial for healthcare professionals to ensure timely and effective patient care. ICU monitors are equipped with advanced alarm systems that alert caregivers to changes in a patient's condition, allowing for prompt intervention. These alarms are categorized into different levels of priority, typically indicated by distinct sounds, colors, or visual displays. High-priority alarms, often denoted by loud, piercing sounds or bright red lights, signal life-threatening conditions that require immediate attention, such as cardiac arrest or severe hypotension. Medium-priority alarms, typically represented by softer sounds or yellow lights, indicate conditions that require prompt attention but are not immediately life-threatening, such as mild hypotension or tachycardia. Low-priority alarms, often signified by gentle sounds or green lights, alert caregivers to non-urgent conditions, such as a patient's oxygen saturation level being slightly below the set threshold. By understanding the alarm system and prioritization on ICU monitors, healthcare professionals can quickly identify the level of urgency and respond accordingly, ensuring that patients receive the necessary care in a timely manner. Effective alarm management is critical in preventing alarm fatigue, which can lead to desensitization and delayed responses to critical alarms. By customizing alarm settings and parameters to individual patient needs, caregivers can minimize unnecessary alarms and optimize the alarm system to provide timely and relevant alerts, ultimately enhancing patient safety and outcomes.