How Long Does It Take For Sperm To Regenerate
 understanding of human health and reproductive ability requires comprehension of myriad intricate processes that happen at a cellular level. One of these fascinating wonders within the male reproductive system is the process of sperm regeneration. In this article, we delve into the fascinating world of sperm production and answer the intriguing question: How long does it take for sperm to regenerate? The upcoming sections will elaborate on the nuanced process allowing our body to continuously produce sperm. First, we will guide you to a comprehensive understanding of sperm regeneration and its biological significance. Next, we focus on the sperm regeneration process itself, unfolding how cells are transformed into potential life-bringers. Finally, we will explore various factors that can affect the efficiency and speed of sperm regeneration. With that broad overview, let's delve into the first section, exploring the fascinating concept of Understanding Sperm Regeneration.
understanding of human health and reproductive ability requires comprehension of myriad intricate processes that happen at a cellular level. One of these fascinating wonders within the male reproductive system is the process of sperm regeneration. In this article, we delve into the fascinating world of sperm production and answer the intriguing question: How long does it take for sperm to regenerate? The upcoming sections will elaborate on the nuanced process allowing our body to continuously produce sperm. First, we will guide you to a comprehensive understanding of sperm regeneration and its biological significance. Next, we focus on the sperm regeneration process itself, unfolding how cells are transformed into potential life-bringers. Finally, we will explore various factors that can affect the efficiency and speed of sperm regeneration. With that broad overview, let's delve into the first section, exploring the fascinating concept of Understanding Sperm Regeneration.Understanding Sperm Regeneration
Human fertility typically revolves around the health and regeneration of sperm, a subject that although vital, is often overlooked. Understanding sperm regeneration can provide crucial insights not only into the biology associated with male reproduction but also shed light on the factors pivotal for the promotion of healthy sperm production. As part of this intricate process, testosterone's role is crucial. This primary male hormone is the lynchpin of sperm production, driving the critical processes that underpin spermatogenesis. Similarly, the impact of age on sperm regeneration cannot be underestimated as it profoundly affects sperm quality and quantity, subsequently influencing fertility outcomes. Yet, our body's functionality isn't solely reliant on inherent bodily mechanisms or ticking biological clocks; it is also impacted by external factors such as nutrition. A balanced diet not only promotes overall health but also significantly contributes to optimal sperm health. In the ensuing sections, we delve deeper into the role of testosterone in sperm production, shedding light on the intricate relationship between these factors and how they underpin the process of sperm regeneration.
1. The Role of Testosterone in Sperm Production
The Role of Testosterone in Sperm Production
Testosterone, commonly known as the 'male hormone', plays an instrumental role in sperm production – a process scientifically termed as spermatogenesis. This hormone, interestingly, isn't merely for developing masculine physical characteristics and maintaining a healthy sex drive, but it is of fundamental and indispensable significance in the context of sperm regeneration. Essentially, the production of sperm commences in the testes – the primary male reproductive organs, also responsible for synthesizing testosterone. The testosterone produced behaves in a dual capacity. To begin with, it stimulates the process of spermatogenesis in the seminiferous tubules, which are discrete compartments within the testes. The Leydig cells, nestled between these tubules, produce testosterone which in turn fosters the development of spermatids into mature, motile sperm cells. The hormone acts as an imperative catalyst, promoting the critical transformations necessary for an immature sperm cell to grow in size, establish a tail, and acquire the ability to independently move- which is essentially vital for fertilization. Moreover, testosterone sustains the numbers of Sertoli cells that are integral in 'nursing' the developing sperm cells. While the correlation between testosterone levels and sperm production cannot be utterly linear due to the influence of other factors, testosterone indisputably plays a potent role. Research indicates that low levels of testosterone, a condition known as hypogonadism, can impair sperm production, often resulting in a lower sperm count. Conversely, extremely high levels due to exogenous testosterone or anabolic steroid use are associated with hampering the hypothalamic-pituitary-gonadal axis, leading to cessation of the endogenous testosterone activity, and ultimately decreasing sperm production. Therefore, maintaining an optimal balance in testosterone levels is essential for adequate sperm production and regeneration. Medical interventions, healthier lifestyle choices, and proper nutrition can help maintain testosterone levels within an ideal range, facilitating the intricate process of sperm production and ensuring robust male fertility. Understanding the intricate relationship between testosterone and sperm production is critical in comprehending the cycle of sperm regeneration. It hints at potential challenges that may affect this essential biological process, ultimately determining male fertility. And, above all, it represents a vital chapter in the broader narrative of human reproduction - a mystery that biological science continues to uncover in many significant ways.
2. The Impact of Age on Sperm Regeneration
The human body is continuously replenishing itself, and sperm regeneration, also known as spermatogenesis, falls within this remit. As a basic biology, a young male starts producing sperm during puberty, it peaks in volume and quality during late teens and gradually wanes after reaching 40. This decline is prominent in context when discussing age's impact on sperm replenishment as it is underlined by the physiologic fact that new sperm takes about 64 days to fully mature in a man's body. One study, commonly recognized within the field, delineates a 0.8% drop in sperm motility per year after age 22, and a decrease in semen volume of 0.03 milliliters per year after age 40. But beyond these volume and motility markers, the central concern is that age can also impact genetic integrity of the sperm. As a man ages, the machinery that replicates DNA can falter, this leads to a higher potential for errors, leading to a surge of genetic mutations that can be passed to offspring. A research conducted by Dr. Allan Pacey, a fertility scientist at the University of Sheffield, found out that a man over 40 is nearly six times more likely to father a child with autism, and twice as likely to have a child with schizophrenia. The increased rate of mutation is due to the DNA duplications that sperm cells go through as a man ages. The genetic research confirms this predisposition. Every year, the cells divisions that sperm undergo allow a new myriad of genetic mutations in the sperm to crop up. Hence, the older the man, the higher the number of cell division in sperm thus the percent of mutated sperm is prevalently higher. The Icelandic deCODE Genetics study provides a fascinating, if disturbing, confirmation that age is a significant factor in the increase in mutations in a man's sperm. Although age presents certain negative impacts on sperm regeneration, it is also worth noting that the decline is gradual and does not typically hinder conception until a man is in his mid-forties. This is not to say that older men cannot father children, but they may face more challenges and potential risks. Furthermore, lifestyle factors such as maintaining a nutritious diet, refraining from smoking or excessive alcohol intake, regular physical activity and managing stress can also have significant positive effects on sperm production and health, thereby mitigating some of the impacts of age. Navigating the process of sperm regeneration as one ages is a matter of understanding these biological facts, acknowledging risks and adopting supportive lifestyle choices. Thus, the quest to longevity and healthy sperm regeneration is a complex matrix of both genetic predisposition and lifestyle adaptations.
3. The Importance of a Balanced Diet for Sperm Health
Healthy nutrition is often a cornerstone for overall well-being, but its impact reach even extends to sperm health. Ensuring a balanced diet is not just important for your general health or to maintain an ideal body weight, but it can dramatically affect your sperm count, their mobility, and overall reproductive ability. Science has shown us that certain deficiencies in the diet – for example, an inadequate intake of specific vitamins and minerals – can lead to lower sperm counts or poor sperm health. For instance, antioxidants such as vitamins C and E, selenium, and coenzyme Q10 are increasingly recognized for their role in protecting sperm from damage. Zinc, on the other hand, has been linked with improving sperm count and motility. However, the role of nutrition in sperm health is not just tied to what you consume, but also what you should avoid. High intakes of processed meats and full-fat dairy products, for instance, have been associated with decreased sperm quality. Similarly, excessive alcohol and caffeine can negatively influence sperm health. Interestingly, research suggests that sperm takes about 74 days to mature, indicating that your nutritional habits two to three months before can impact your current sperm health. Therefore, adapting a well-rounded, balanced diet that is low in processed food and high in antioxidants, lean proteins, fruits, and vegetables not only boosts general health but plays a pivotal role in sperm health and regeneration. It is also recommended to maintain a healthy weight, as overweight and obesity have been linked with lower sperm count and impaired sperm function. In conclusion, maintaining a balanced diet is not just about restoring balance in your body, but it also reflects the health of your sperm. Consuming nutrient-rich foods and eliminating harmful dietary habits will not only improve your overall health but also optimize your sperm health, counting towards a successful conception. In this light, understanding the importance of a balanced diet for sperm health becomes crucial as it is a key supporting factor for efficient and healthy sperm regeneration.
The Sperm Regeneration Process
Science's understanding of the male reproductive system has deepened significantly over time, leading to the discovery of the incredible and complex process of sperm regeneration. Gaining insight into this procedure is crucial given its crucial function in procreation and overall male health. In the subsequent portions of the article, we will discuss the sperm regeneration process in greater detail. Beginning with the spermatogenesis cycle and its duration, this process is the lynchpin for ensuring the constant supply of healthy sperm. Following this, we will explore the pivotal role hormones play in regulating sperm production, something that biological procedures cannot accomplish without. Thirdly, we will delve into the often overlooked effects of stress on sperm regeneration, an element of our daily lives which can significantly impact this intricate process. These three facets will work in concert to offer a comprehensive understanding of the sperm regeneration journey. Now, let's shift our focus to the fascinating spermatogenesis cycle and its duration, a realm where the magic of the regenerative process really begins.
1. The Spermatogenesis Cycle and Its Duration
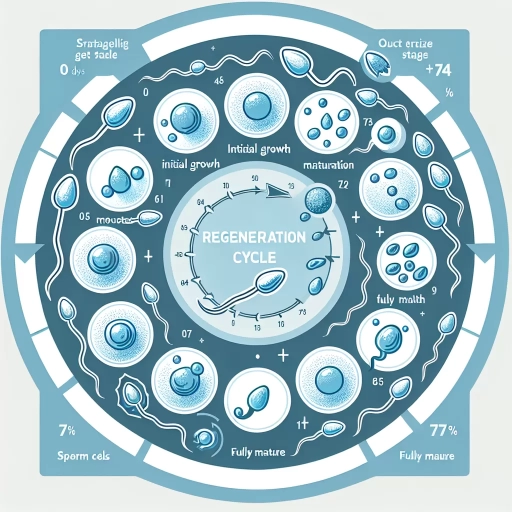
Spermatogenesis, the cycle through which sperm is developed, is a complex but crucial process in male reproduction. It's a recurrent cycle that not only produces millions of sperm each day but also ensures the genetic diversity necessary for species survival. The spermatogenesis cycle, which typically spans approximately 64 to 72 days, is divided into three main stages: spermatocytogenesis, spermatidogenesis, and spermiogenesis. Spermatocytogenesis, also known as germ cell proliferation, is the first stage in which the primitive germ cells, called spermatogonia, divide and differentiate into primary spermatocytes through a process known as mitosis. This phase takes around 24 days. In the second stage, spermatidogenesis, these primary spermatocytes undergo two successive rounds of cell division called meiosis I and II, producing spermatids. This phase lasts approximately 24 days as well. Finally, during the spermiogenesis stage, spermatids are transformed into mature spermatozoa, more commonly known as sperm, in a process that lasts about 16 days. This transformation includes a series of morphological changes, such as the formation of an acrosomal cap, condensation of the nucleus, formation of the tail, and subsequent release of the sperm into the lumen of seminiferous tubule, known as spermiation. Once spermiation occurs, the sperm travel into the epididymis, where they undergo further maturation and acquire motility and fertility capabilities, a process that takes another seven to ten days. Thus, the entire sperm development process from spermatogonia to fully mature sperm takes about two to two and a half months on average. Although the spermatogenesis cycle is a continuous process that produces millions of sperm daily, it's crucial to also consider the sperm regeneration process or spermiogenesis. This process allows a sustained production of male gametes without depleting the pool of spermatogonia. As an integral part of the sperm production process, understanding spermatogenesis and its duration can provide insights into male fertility and potential causes and treatments of infertility. Hence, spermatogenesis, the cycle responsible for the production of sperm, plays an essential role in the reproduction process. Its duration allows the maintenance of the delicate balance necessary for the continuous and efficient production of sperm, with intricate stages each playing significant roles in ensuring the correct formation, maturation, and delivery of healthy, viable sperm.
2. The Role of Hormones in Regulating Sperm Production
of reproductive biology, the role of hormones in controlling sperm production, an element of the sperm regeneration process, is a complex and fascinating aspect. Hormones coordinate a multitude of functions within the body, from our growth and metabolism to our reactions to stress. However, in the context of male fertility, they gain additional significance as key components in the production and regulation of sperm. The sperm regeneration process is largely governed by two principal hormones: Follicle-stimulating hormone (FSH) and Luteinizing hormone (LH). FSH triggers the production of sperm by activating the Sertoli cells within the testes, which offer nourishment and support to developing sperm cells. Meanwhile, LH stimulates the Leydig cells, also found within the testes, to secrete testosterone – an essential hormone for sperm production. One significant factor is the intricately coordinated process of the hypothalamic-pituitary-gonadal (HPG) axis. The HPG axis is a hormonal system involving the hypothalamus, pituitary gland, and the gonads (testes in males). This axis regulates the production and release of hormones in a complex loop of feedback mechanisms. The hypothalamus secretes gonadotropin-releasing hormone (GnRH), which then signals the pituitary gland to release FSH and LH into the bloodstream. These hormones further stimulate the testes to produce testosterone and initiate sperm production. The introduction of hormones, however, is just the first step. Understanding the underlying process of spermatogenesis relies on realizing the vital role of these hormones. Spermatogenesis is the process by which spermatozoa, or mature sperm cells, are produced in the testes. It's a multi-staged process that begins with a spermatogonium (immature sperm cell) and ends with a mature, motile spermatozoon. This process, controlled largely by FSH, LH, and testosterone, ensures the production of healthy, fertile sperm capable of fertilizing an egg cell. Moreover, research has suggested that insulin-like growth factor-1 (IGF-1), another hormone, may play a crucial role in regulating sperm production and promoting spermatogenesis by enhancing the actions of FSH and testosterone. IGF-1 is primarily produced in the liver and is known to regulate cell growth and development in almost every cell in the body. In conclusion, our grasp of the complex process of sperm regeneration is deepened through understanding the role of hormones. The interconnected hormonal mechanisms involving FSH, LH, testosterone, and potentially IGF-1 demonstrate a fascinating and intricate example of how our bodies maintain and regulate essential physiological processes. As part of the broader topic of understanding how long it takes for sperm to regenerate, the significance of hormones certainly cannot be underestimated. They provide a key to unlock insights into male fertility, with potential implications for diagnosing and treating reproductive health problems.
3. The Effects of Stress on Sperm Regeneration
Recent scientific research has posited that stress, regardless of whether it is physical or psychological, can have a considerable impact on the process of sperm regeneration. One of the most profound effects is a decrease in semen volume or quality, which can lead to difficulty while trying to conceive. When a male body is subjected to prolonged stress, the adrenal glands produce an excessive amount of the hormone cortisol, which can disrupt the fine hormonal balance required for the production of sperm. Essentially, cortisol inhibits the release of Gonadotropin-releasing hormone (GnRH) from the hypothalamus, leading to a decline in the production of testosterone, a hormone crucial to the process of spermatogenesis. This stress-induced cortisol kicks off a hormonal avalanche that limits the production of sperm by restraining other hormones essential for spermatogenesis, such as follicle-stimulating hormone (FSH) and luteinizing hormone (LH). The downstream effects of this situation translate into a reduced number of sperm cells, reduced sperm motility, and troubled sperm morphology - all crucial factors that determine the quality of sperm. Moreover, stress also stimulates the sympathetic nervous system, eliciting the ‘fight or flight’ response. As a result, the body prioritizes survival over processes like sperm regeneration. In the long term, this might lead to a dysfunction in the release of sperm and semen - a condition referred to as an ejaculation disorder. Additionally, stressed individuals often exhibit unhealthy habits such as poor dietary choices, irregular sleep patterns, abuse of substances like alcohol and drugs, and lack of physical exercise. These lifestyle habits can exacerbate the situation, resulting in decreased sperm count and fertility issues. While short term stress is a normal part of life and unlikely to affect sperm regeneration dramatically, chronic or long term stress might have a significant impact on sperm production and fertility. It is essential to manage stress effectively through healthy lifestyle choices, therapies like mindfulness or cognitive-behavioral therapy, and maintaining a supportive social network to ensure good sexual health and fertility. Incorporating these remedies into their lives, men can mitigate the impact of stress on their sperm regeneration process, ensuring healthier and more potent sperm. In the grand scheme of things, understanding the role of stress in sperm regeneration provides critical insight into the multiple dimensions that determine male fertility - a topic that often stays overlooked in discourses around reproductive health. Moreover, it draws greater attention to the importance of mental health and stress management, not just in the context of fertility but overall wellbeing. It also encourages the design of more holistic interventions and therapies to enhance male fertility and the overall reproductive health landscape.
Factors Affecting Sperm Regeneration
Sperm regeneration is a complex biological process that is influenced by a wide range of factors, some of which males have direct control over, and others that are dictated by surrounding conditions. Crucially, men must understand these factors to take necessary measures to maintain a healthy reproductive system or optimize their chances of procreation. This article will explore in depth three primary aspects that play an integral role in this intricate process. Firstly, the impact of environmental toxins on sperm health, testifying the perilous implications of chemical exposures. The second segment will delve into the role of individual lifestyle choices in sperm regeneration, identifying the detrimental effect of unhealthy habits and the importance of making lifestyle amends where necessary. Lastly, this discourse throws light on how certain medical conditions could adversely impact sperm production. As we navigate through these complex layers, it becomes evident that sperm health isn't merely restricted to a man's physical condition, but is also significantly shaped by his surroundings, lifestyle, and overarching health. Elaborating on this, let's commence by examining the profound impact environmental toxins have on sperm health.
1. The Impact of Environmental Toxins on Sperm Health
The impact of environmental toxins on sperm health forms a critical aspect under the broad topic of factors affecting sperm regeneration. Several studies now confirm that the quality and the regeneration of sperm can be heavily influenced by exposure to environmental toxins, underlining the significant role environmental factors play in male fertility. These environmental toxins, also classified as endocrine disruptors, include a diverse range of chemicals like pesticides, metals, air pollutants, and industrial chemicals, many of which are impossible to avoid in our daily lives. Research spanning multiple decades reveals a concerning decline in men’s sperm count, with environmental toxins being identified as a significant contributing factor. In particular, these toxins can affect sperm counts, motility, morphology, and overall sperm health. One such example is Phthalates – a group of chemicals used in hundreds of products from plastics to cosmetics, which studies suggest are associated with poor sperm quality and reduction in the anogenital distance in males – a marker linked to infertility. Additionally, heavy metals such as lead, arsenic, and cadmium are also major culprits affecting sperm health. These metals, prevalent in occupational settings, can negatively affect sperm count, motility, and cause DNA damage. Air pollutants are not innocent bystanders either in this context. For instance, exposure to fine particulate matter (PM2.5), a common air pollutant, has shown associations with reduced sperm quality. Various other industrial chemicals like Bisphenol A, primarily found in polycarbonate plastics and epoxy resins used in food and beverage packaging, are of grave concern too. Even low-dose exposure to Bisphenol A has been linked to poor semen quality and potential fertility impairment. Moreover, persistent organic pollutants like polychlorinated biphenyls and organochlorine pesticides, despite being banned in many countries, continue to linger in the environment, posing added risks to sperm health. Strikingly, these toxins do not merely affect the exposed individual but can also impact the health and fertility of future generations, as sperm carry the potential to transmit environmentally induced conditions to offspring. The damage caused by these toxins underscores the need for increased awareness and proactive measures to reduce exposure. This may include lifestyle modifications, occupational safety measures, or even regulatory steps on a broader scale to reduce the prevalence of these toxins in our environment. In conclusion, environmental toxins present a tangible threat to sperm health and regeneration, thereby playing a significant role in male fertility. Their widespread presence underscores the need for urgent attention in the realms of both research and public health policy.
2. The Role of Lifestyle Choices in Sperm Regeneration
The role of lifestyle choices in sperm regeneration cannot be overstated as they significantly influence sperm production and overall male fertility. Maintaining a healthy lifestyle can improve sperm regeneration, leading to increased fertility and optimal reproductive health. This involves key choices such as diet, exercise, sleep, avoidance of harmful substances, stress management, and maintaining an appropriate body weight. Nutrition plays a vital role in sperm production - a diet rich in antioxidants, vitamins, and minerals can boost sperm health. Consuming high-quality proteins, fresh fruits and vegetables, whole grains, and healthy fats such as omega-3 fatty acids found in fish can significantly enhance sperm quality. Furthermore, regular physical activity and exercise have been shown to improve sperm count and motility, with sessions of moderate intensity being the most beneficial. Sleep is another crucial component; studies have linked sleep disturbances with lower testosterone levels, contributing to decreased sperm count. Hence, having a proper sleep schedule is critical for optimum sperm regeneration. There is a robust unanimity among researchers about the detrimental effects of substances like alcohol, tobacco, and illicit drugs on male fertility. These factors contribute to oxidative stress, DNA damage, reduced sperm count, and impaired sperm motility. Thus, abstaining from these substances or reducing their intake can greatly enhance sperm regeneration. Chronic stress also interferes with hormones needed for sperm production. So, managing stress through mindfulness, meditation, yoga, or other relaxation techniques can be beneficial. Additionally, being overweight or obese has been linked to lower sperm count and poorer sperm quality. Maintaining healthy body weight through balanced diet and exercise can thus support sperm regeneration. In conclusion, lifestyle choices exert a profound influence on sperm regeneration. Therefore, adopting a healthy lifestyle is crucial for boosting sperm production and enhancing male fertility. Emphasizing wholesome nutrition, regular physical activity, adequate sleep, avoidance of harmful substances, stress management, and maintaining a healthy weight can contribute significantly to improved sperm health and regeneration. This, in turn, can increase the chances of successful conception, emphasizing the vital role that lifestyle choices play in male reproductive health. It is, therefore, clear that these factors are invaluable in maintaining the efficacy of the sperm regeneration process.
3. The Effects of Medical Conditions on Sperm Production
The Effect of Medical Conditions on Sperm Production Many medical conditions can pose a significant impact on sperm production, thereby affecting sperm regeneration time. The first common condition is Varicocele, affecting about 15% of men overall and up to 40% of infertile men. It is characterized by the enlargement of the veins within the loose bag of skin that holds your testicles (scrotum), causing a decrease in sperm count and a decline in sperm quality. The decrease in sperm number and quality is due to varicocele's tendency to raise the temperature in the testicles, disrupting optimal conditions for sperm production. Another common medical condition that affects sperm production is infection and diseases. Sexually transmitted diseases (STDs) like Gonorrhea or HIV, recurrent urinary tract infections, or prostatitis can reduce sperm count significantly. Diverse infections can cause the scarring that blocks the passage of sperm. Hormonal imbalances, including conditions such as hypogonadism, hyperthyroidism, and hypothyroidism, may also contribute to a reduced sperm count. Hormones produced by the pituitary gland are responsible for stimulating the testicles to produce sperm. Any changes or diseases affecting the pituitary gland or the hormonal pathway can thereby diminish sperm production capacity. Cancer and cancer treatments, including radiation, chemotherapy, and surgery, can also significantly change sperm production. Radiation therapy and chemotherapy can severely decrease sperm production by damaging the cells responsible for sperm generation. Sometimes, this reduction is temporary, but it can also be permanent. Lastly, conditions that lead to ejaculation issues can also affect sperm production. Conditions such as diabetes, spinal injuries, medications, and surgery of the bladder, prostate or urethra can lead to retrograde ejaculation. This condition occurs when semen enters the bladder instead of emerging through the penis during orgasm. Though one still reaches sexual climax, little to no semen is ejaculated. This significantly reduces the number of sperms that can be available for fertilization. In summary, different medical conditions can tremendously affect sperm production directly or indirectly, some resulting in irreversible infertility issues. Recognizing the impact these conditions can have on fertility is essential for early intervention and treatment. Thus, men with these conditions or experiencing any symptoms related to these conditions should consult a medical professional for a comprehensive fertility evaluation.