How Long Does It Take For Metformin To Work
Metformin is a widely prescribed medication for managing type 2 diabetes, but many patients are left wondering how long it takes for the drug to start working. The answer to this question is not straightforward, as it depends on several factors, including the individual's health status, dosage, and response to the medication. To understand how long it takes for metformin to work, it's essential to delve into the drug's mechanism of action, the factors that influence its onset of effects, and the timeline for noticing its benefits. By exploring these aspects, patients can gain a better understanding of what to expect from metformin treatment. In this article, we will first explore Understanding Metformin's Mechanism of Action, which is crucial in grasping how the drug works and why it takes time to produce noticeable effects.
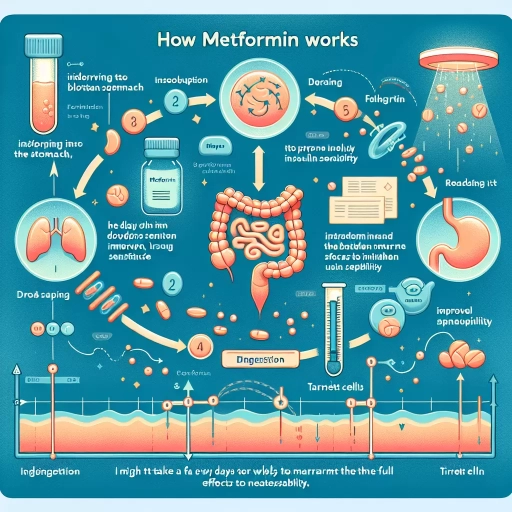
Understanding Metformin's Mechanism of Action
Metformin is a widely prescribed oral antidiabetic drug in the biguanide class that is primarily used for the treatment of type 2 diabetes. To understand how metformin works, it is essential to delve into its mechanism of action, which involves multiple pathways that ultimately lead to improved glycemic control. One of the primary ways metformin exerts its effects is by enhancing insulin sensitivity, allowing glucose to enter cells more efficiently. Additionally, metformin has been shown to decrease glucose production in the liver, reducing the amount of glucose released into the bloodstream. Furthermore, metformin has been found to aid in weight loss and appetite suppression, which can also contribute to improved blood sugar control. By examining metformin's effect on insulin sensitivity, its impact on glucose production in the liver, and its role in weight loss and appetite suppression, we can gain a deeper understanding of how this medication works to manage type 2 diabetes. Let's start by exploring metformin's effect on insulin sensitivity.
Metformin's Effect on Insulin Sensitivity
Metformin's effect on insulin sensitivity is a crucial aspect of its mechanism of action. By activating the AMP-activated protein kinase (AMPK) pathway, metformin increases the body's sensitivity to insulin, allowing glucose to enter cells more efficiently. This, in turn, reduces the amount of glucose produced by the liver and decreases the body's reliance on insulin. As a result, metformin has been shown to improve insulin sensitivity in both diabetic and non-diabetic individuals, making it an effective treatment for type 2 diabetes and a potential therapeutic agent for other insulin-resistant conditions. Furthermore, metformin's ability to enhance insulin sensitivity has been linked to its anti-inflammatory and antioxidant properties, which may also contribute to its beneficial effects on cardiovascular health. Overall, metformin's impact on insulin sensitivity is a key factor in its ability to regulate blood sugar levels and improve metabolic health.
Metformin's Impact on Glucose Production in the Liver
Metformin's impact on glucose production in the liver is a crucial aspect of its mechanism of action. By inhibiting the enzyme glucose-6-phosphatase, metformin reduces the liver's ability to produce glucose through gluconeogenesis. This decrease in glucose production leads to a reduction in the amount of glucose released into the bloodstream, ultimately lowering blood sugar levels. Furthermore, metformin also increases the sensitivity of the liver to insulin, allowing glucose to be more efficiently taken up by the liver and stored as glycogen. This dual action of metformin on the liver not only decreases glucose production but also enhances glucose uptake, making it an effective treatment for type 2 diabetes. Additionally, metformin's effects on the liver have also been shown to improve insulin sensitivity and reduce inflammation, which can help to mitigate the risk of cardiovascular disease and other complications associated with diabetes. Overall, metformin's impact on glucose production in the liver is a key component of its therapeutic benefits, and its ability to modulate liver function has made it a cornerstone of diabetes treatment.
Metformin's Role in Weight Loss and Appetite Suppression
Metformin, a widely prescribed medication for type 2 diabetes, has been found to have a significant impact on weight loss and appetite suppression. Studies have consistently shown that metformin can lead to a reduction in body weight, particularly in individuals with insulin resistance and obesity. The exact mechanisms by which metformin promotes weight loss are not fully understood, but several theories have been proposed. One theory is that metformin decreases glucose production in the liver, leading to a reduction in insulin levels and an increase in the body's sensitivity to insulin. This, in turn, can lead to a decrease in hunger and an increase in feelings of fullness, resulting in reduced caloric intake. Additionally, metformin has been shown to increase the production of certain hormones, such as peptide YY and glucagon-like peptide-1, which are involved in appetite regulation. Furthermore, metformin has been found to have a positive effect on gut health, increasing the production of beneficial gut bacteria and reducing inflammation, which can also contribute to weight loss. Overall, the combination of metformin's effects on insulin sensitivity, appetite regulation, and gut health make it a valuable tool for weight loss and appetite suppression, particularly in individuals with type 2 diabetes or insulin resistance.
Factors Influencing the Onset of Metformin's Effects
Metformin is a widely prescribed medication for the treatment of type 2 diabetes, and its effectiveness is influenced by several factors. One of the key considerations is the dosage and titration of the medication, as this can significantly impact the onset of its effects. Additionally, individual variability in response to metformin can also play a crucial role in determining when its effects become apparent. Furthermore, lifestyle factors such as diet and exercise can also influence the efficacy of metformin, and thus, its onset of action. Understanding these factors is essential for healthcare providers to optimize metformin therapy and achieve the best possible outcomes for their patients. In this article, we will explore the factors that influence the onset of metformin's effects, starting with the impact of dosage and titration on the medication's efficacy.
Dosage and Titration: How They Affect the Onset of Action
The dosage and titration of metformin play a significant role in determining the onset of action. The standard starting dose of metformin is 500-1000 mg per day, taken orally with meals to minimize gastrointestinal side effects. However, the dosage may be adjusted based on individual patient needs and response to treatment. Titration, or the gradual increase in dosage, is often used to minimize side effects and improve tolerability. A common titration schedule involves increasing the dose by 500 mg every 1-2 weeks, up to a maximum dose of 2000-2500 mg per day. The onset of action for metformin is typically seen within 1-2 weeks after initiation of treatment, with maximal effects observed after 2-3 months. However, the rate of onset can be influenced by factors such as the dosage and titration schedule, as well as individual patient characteristics. For example, patients with more severe insulin resistance may require higher doses or more rapid titration to achieve optimal effects. In contrast, patients with milder insulin resistance may experience a more rapid onset of action with lower doses. Overall, the dosage and titration of metformin are critical factors in determining the onset of action, and should be carefully individualized to optimize treatment outcomes.
Individual Variability in Metformin Response
Metformin's efficacy can vary significantly from person to person, a phenomenon known as individual variability in metformin response. This variability can be attributed to several factors, including genetic differences, body composition, and the presence of comorbidities. For instance, individuals with a higher body mass index (BMI) may require higher doses of metformin to achieve the same level of glucose control as those with a lower BMI. Additionally, genetic variations in the genes involved in metformin's mechanism of action, such as the SLC22A1 gene, can affect the drug's efficacy and tolerability. Furthermore, the presence of comorbidities like kidney disease or liver disease can impact metformin's pharmacokinetics and pharmacodynamics, leading to variable responses. As a result, healthcare providers must carefully consider these individual factors when prescribing metformin and monitoring its effects to ensure optimal glucose control and minimize adverse effects.
The Impact of Diet and Exercise on Metformin's Efficacy
The efficacy of metformin can be significantly influenced by diet and exercise. A healthy diet that is low in sugar, refined carbohydrates, and saturated fats can enhance the effects of metformin, while a diet high in these substances can hinder its efficacy. Regular exercise, such as cardio and strength training, can also improve insulin sensitivity, which can increase the effectiveness of metformin. Studies have shown that patients who combine metformin with a healthy diet and regular exercise experience greater improvements in blood sugar control and weight loss compared to those who take the medication alone. Furthermore, a diet rich in fiber, vitamins, and minerals can help to mitigate the gastrointestinal side effects of metformin, such as diarrhea and nausea. Overall, a healthy lifestyle that includes a balanced diet and regular physical activity can optimize the effects of metformin and improve overall health outcomes.
Timeline for Noticing Metformin's Effects
Metformin is a widely prescribed medication for managing type 2 diabetes, and its effects can vary significantly from person to person. When starting metformin, it's essential to understand the timeline of its effects to manage expectations and monitor progress effectively. In this article, we'll explore the timeline of metformin's effects, including short-term effects that can be expected in the first few weeks, medium-term effects that become apparent after 2-3 months of treatment, and long-term effects that can be observed after 6 months or more. By understanding this timeline, individuals can better navigate the treatment process and work closely with their healthcare provider to achieve optimal results. In the first few weeks of taking metformin, individuals can expect to experience some initial side effects, which can be a sign that the medication is starting to take effect. Let's take a closer look at what to expect during this initial period.
Short-Term Effects: What to Expect in the First Few Weeks
When starting metformin, it's essential to understand the short-term effects you may experience in the first few weeks. Within the initial 1-2 weeks, you may notice a decrease in blood sugar levels, which can lead to improved insulin sensitivity. This is because metformin works by reducing glucose production in the liver and increasing insulin sensitivity in the body. As a result, you may experience a reduction in symptoms such as increased thirst and urination, fatigue, and blurred vision. However, some people may experience gastrointestinal side effects like diarrhea, nausea, and stomach cramps, which are usually mild and temporary. These side effects often subside within 2-4 weeks as your body adjusts to the medication. Additionally, metformin can cause a metallic taste in the mouth, which can be unpleasant but is generally not a cause for concern. It's also common to experience weight loss, particularly in the first few weeks, as metformin can help reduce appetite and increase feelings of fullness. Overall, the short-term effects of metformin can vary from person to person, but most people can expect to start noticing improvements in their blood sugar control and overall health within the first few weeks of treatment.
Medium-Term Effects: Changes After 2-3 Months of Treatment
After 2-3 months of metformin treatment, several changes become noticeable. One of the primary effects is the improvement in insulin sensitivity, which allows glucose to enter the cells more efficiently, reducing blood sugar levels. As a result, hemoglobin A1c (HbA1c) levels, which reflect average blood sugar control over the past 2-3 months, begin to decrease. This reduction in HbA1c levels is a significant indicator of the medication's effectiveness. Additionally, metformin's ability to decrease glucose production in the liver becomes more pronounced, leading to lower fasting blood sugar levels. Furthermore, metformin's impact on weight loss becomes more apparent, as it helps reduce hunger and increase feelings of fullness, leading to a decrease in body weight. Overall, the medium-term effects of metformin treatment are characterized by improved insulin sensitivity, reduced blood sugar levels, and weight loss, all of which contribute to better management of type 2 diabetes.
Long-Term Effects: Metformin's Impact After 6 Months or More
Metformin's long-term effects become more pronounced after 6 months or more of consistent use. At this stage, the medication has had sufficient time to exert its full impact on the body, leading to significant improvements in insulin sensitivity, glucose metabolism, and weight management. Studies have shown that metformin's efficacy in reducing HbA1c levels, a marker of average blood sugar control, continues to increase over time, with the greatest reductions observed after 12-18 months of treatment. Additionally, long-term metformin use has been associated with a lower risk of cardiovascular events, such as heart attacks and strokes, as well as a reduced risk of developing certain types of cancer, including breast and colon cancer. Furthermore, metformin's anti-inflammatory properties may also contribute to its long-term benefits, as chronic inflammation is a known risk factor for many diseases. Overall, the long-term effects of metformin are a testament to its effectiveness as a treatment for type 2 diabetes and its potential to improve overall health outcomes.