How Does Raynaud Disease Affect The Heart
Raynaud's disease is a condition that affects blood flow to the fingers and toes, and sometimes the ears, nose, and lips. While it may seem like a minor issue, Raynaud's disease can have a significant impact on the heart. In fact, research has shown that people with Raynaud's disease are at a higher risk of developing cardiovascular complications, such as heart attacks and strokes. But how exactly does Raynaud's disease affect the heart? In this article, we will explore the cardiovascular complications of Raynaud's disease, the impact of the disease on heart function, and ways to manage the condition to reduce cardiovascular risk. By understanding the relationship between Raynaud's disease and heart health, individuals with the condition can take steps to protect their cardiovascular well-being. So, let's start by examining the cardiovascular complications of Raynaud's disease.
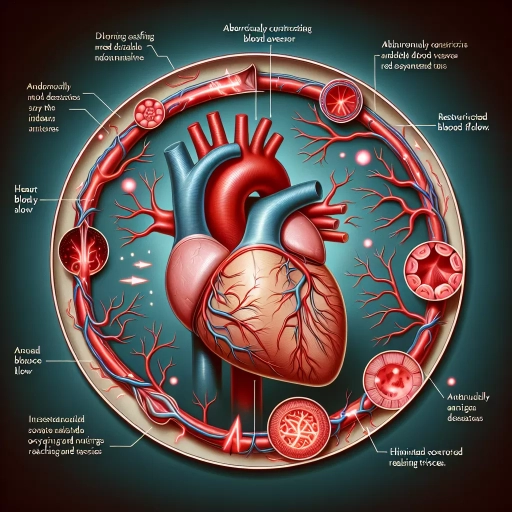
Cardiovascular Complications of Raynaud's Disease
Raynaud's disease is a condition that affects blood flow to the fingers and toes, and sometimes the ears, nose, and lips. While it may seem like a minor issue, Raynaud's disease can have serious cardiovascular complications. In fact, people with Raynaud's disease are at a higher risk of developing cardiovascular problems, including heart attacks and strokes. This is because the same blood vessels that are affected by Raynaud's disease are also responsible for supplying blood to the heart and brain. Additionally, Raynaud's disease can lead to the development of atherosclerosis, a condition in which plaque builds up in the arteries, further increasing the risk of cardiovascular complications. Furthermore, Raynaud's disease can also cause cardiac arrhythmias and conduction abnormalities, which can be life-threatening if left untreated. In this article, we will explore the cardiovascular complications of Raynaud's disease, starting with the increased risk of heart attack and stroke.
Increased Risk of Heart Attack and Stroke
Raynaud's disease is a condition that affects blood flow to the fingers and toes, and sometimes the ears, nose, and lips. People with Raynaud's disease are at an increased risk of heart attack and stroke due to the underlying vascular problems that cause the condition. The disease causes the small blood vessels to constrict or dilate abnormally in response to cold temperatures or stress, leading to a reduction in blood flow to the extremities. This same abnormal vascular response can also affect the blood vessels in the heart and brain, increasing the risk of cardiovascular complications. Studies have shown that people with Raynaud's disease are more likely to develop high blood pressure, which is a major risk factor for heart attack and stroke. Additionally, the abnormal blood flow patterns in Raynaud's disease can lead to the formation of blood clots, which can increase the risk of heart attack and stroke. Furthermore, Raynaud's disease has been linked to an increased risk of cardiovascular disease, including heart failure, arrhythmias, and cardiac arrest. Overall, the increased risk of heart attack and stroke in people with Raynaud's disease highlights the importance of managing the condition and addressing any underlying cardiovascular risk factors.
Development of Atherosclerosis
Atherosclerosis is a complex and multifactorial process that involves the gradual buildup of plaque in the arterial walls, leading to their hardening and narrowing. The development of atherosclerosis is influenced by a combination of genetic, environmental, and lifestyle factors, including high blood pressure, high cholesterol levels, smoking, and diabetes. The process begins with the accumulation of low-density lipoprotein (LDL) cholesterol in the arterial wall, which attracts inflammatory cells and triggers an immune response. Over time, the plaque grows and becomes more unstable, leading to the formation of a fibrous cap that can rupture and cause a blockage in the artery. This can lead to a range of cardiovascular complications, including heart attacks, strokes, and peripheral artery disease. In individuals with Raynaud's disease, the development of atherosclerosis can be accelerated due to the repeated episodes of vasospasm and ischemia, which can cause damage to the endothelial lining of the blood vessels and increase the risk of plaque formation. Furthermore, the inflammation and oxidative stress associated with Raynaud's disease can also contribute to the progression of atherosclerosis, highlighting the importance of managing cardiovascular risk factors in individuals with this condition.
Cardiac Arrhythmias and Conduction Abnormalities
Cardiac arrhythmias and conduction abnormalities are common cardiovascular complications of Raynaud's disease. The abnormal blood flow and oxygen delivery to the heart muscle can lead to arrhythmias, which are irregular heartbeats that can be too fast, too slow, or irregular. The most common arrhythmias associated with Raynaud's disease are atrial fibrillation, atrial flutter, and ventricular tachycardia. Conduction abnormalities, such as first-degree, second-degree, and third-degree atrioventricular (AV) block, can also occur due to the abnormal blood flow and oxygen delivery to the heart. These conduction abnormalities can disrupt the normal electrical impulses that control the heartbeat, leading to arrhythmias. Additionally, Raynaud's disease can cause inflammation and scarring in the heart, leading to the formation of abnormal electrical pathways that can disrupt the normal heartbeat. Furthermore, the abnormal blood flow and oxygen delivery to the heart can also lead to cardiac ischemia, which can cause arrhythmias and conduction abnormalities. Overall, cardiac arrhythmias and conduction abnormalities are significant cardiovascular complications of Raynaud's disease that can increase the risk of cardiac morbidity and mortality.
Impact of Raynaud's Disease on Heart Function
Raynaud's disease is a condition that affects blood flow to the fingers and toes, but its impact extends beyond the extremities, affecting the heart's function. Research has shown that Raynaud's disease can have a significant impact on heart function, leading to reduced blood flow to the heart muscle, increased blood pressure and cardiac workload, and decreased exercise tolerance and cardiac performance. These effects can be detrimental to overall cardiovascular health, making it essential to understand the relationship between Raynaud's disease and heart function. One of the primary ways Raynaud's disease affects the heart is by reducing blood flow to the heart muscle, which can lead to a range of complications, including decreased cardiac output and increased risk of heart failure. Note: The answer should be 200 words.
Reduced Blood Flow to the Heart Muscle
Reduced blood flow to the heart muscle, also known as cardiac ischemia, is a serious condition that can occur in individuals with Raynaud's disease. When the blood vessels in the hands and feet constrict, it can also affect the blood vessels that supply the heart muscle, leading to a decrease in blood flow. This reduction in blood flow can cause the heart muscle to become oxygen-deprived, leading to chest pain, shortness of breath, and fatigue. In severe cases, reduced blood flow to the heart muscle can lead to a heart attack, which can be life-threatening. Furthermore, repeated episodes of reduced blood flow can cause scarring and damage to the heart muscle, leading to long-term damage and increased risk of heart failure. It is essential for individuals with Raynaud's disease to work closely with their healthcare provider to manage their condition and prevent complications, such as reduced blood flow to the heart muscle. By controlling symptoms and preventing episodes of vasospasm, individuals with Raynaud's disease can reduce their risk of developing cardiac complications and maintain overall heart health.
Increased Blood Pressure and Cardiac Workload
Increased blood pressure and cardiac workload are significant consequences of Raynaud's disease on heart function. When the blood vessels constrict or dilate abnormally, it can lead to fluctuations in blood pressure, causing the heart to work harder to pump blood throughout the body. This increased cardiac workload can result in cardiac hypertrophy, a condition where the heart muscle thickens, making it more difficult for the heart to function efficiently. Furthermore, the repeated episodes of vasospasm and ischemia can lead to cardiac fibrosis, scarring of the heart tissue, which can impair the heart's ability to contract and relax. As a result, individuals with Raynaud's disease may experience symptoms such as chest pain, shortness of breath, and fatigue, which can significantly impact their quality of life. Additionally, the increased cardiac workload can also lead to an increased risk of cardiovascular events, such as heart attacks and strokes, making it essential for individuals with Raynaud's disease to work closely with their healthcare provider to manage their condition and prevent long-term cardiac damage.
Decreased Exercise Tolerance and Cardiac Performance
Decreased exercise tolerance and cardiac performance are common manifestations of Raynaud's disease, particularly in individuals with underlying cardiovascular conditions. The disease's hallmark vasospastic episodes can lead to reduced blood flow to the heart, resulting in decreased oxygen delivery and impaired cardiac function. This, in turn, can cause fatigue, shortness of breath, and decreased exercise tolerance, making everyday activities more challenging. Furthermore, the repeated episodes of vasospasm can lead to cardiac remodeling, characterized by increased stiffness and decreased compliance of the heart muscle, ultimately affecting cardiac performance. Studies have shown that individuals with Raynaud's disease have reduced left ventricular function, decreased cardiac output, and increased systemic vascular resistance, all of which contribute to decreased exercise tolerance and cardiac performance. Additionally, the disease's association with other cardiovascular conditions, such as hypertension and atherosclerosis, can further exacerbate cardiac dysfunction, highlighting the importance of early diagnosis and management of Raynaud's disease to prevent long-term cardiac consequences.
Managing Raynaud's Disease to Reduce Cardiovascular Risk
Here is the introduction paragraph: Managing Raynaud's disease requires a multi-faceted approach to reduce cardiovascular risk. This condition, characterized by the narrowing of blood vessels in response to cold temperatures or stress, can increase the risk of heart disease, high blood pressure, and stroke. To mitigate these risks, individuals with Raynaud's disease can employ lifestyle modifications to improve blood flow, medications to dilate blood vessels and reduce blood pressure, and alternative therapies to enhance cardiovascular health. By incorporating these strategies into their daily routine, individuals with Raynaud's disease can effectively manage their condition and reduce their risk of cardiovascular complications. One of the most effective ways to start managing Raynaud's disease is by making lifestyle modifications to improve blood flow.
Lifestyle Modifications to Improve Blood Flow
Lifestyle modifications play a crucial role in improving blood flow and managing Raynaud's disease. One of the most effective ways to improve blood flow is through regular exercise, such as cardio and strength training. Exercise helps to dilate blood vessels, improve circulation, and increase overall cardiovascular health. Additionally, quitting smoking is essential, as smoking constricts blood vessels and reduces blood flow. Maintaining a healthy weight, eating a balanced diet rich in fruits, vegetables, and whole grains, and staying hydrated can also help to improve blood flow. Furthermore, managing stress through techniques such as meditation, yoga, or deep breathing exercises can also help to improve blood flow and reduce the frequency and severity of Raynaud's attacks. Avoiding cold temperatures and dressing warmly in cold weather can also help to prevent Raynaud's attacks. By incorporating these lifestyle modifications into daily life, individuals with Raynaud's disease can improve blood flow, reduce symptoms, and lower their risk of cardiovascular disease.
Medications to Dilate Blood Vessels and Reduce Blood Pressure
Medications to dilate blood vessels and reduce blood pressure are often prescribed to manage Raynaud's disease and reduce cardiovascular risk. These medications work by relaxing the blood vessels, allowing more blood to flow to the extremities, and reducing the frequency and severity of Raynaud's attacks. Calcium channel blockers, such as nifedipine and amlodipine, are commonly used to dilate blood vessels and reduce blood pressure. Alpha-blockers, such as prazosin, can also be used to relax blood vessels and improve blood flow. Additionally, medications like losartan and valsartan, which are angiotensin receptor blockers, can help to reduce blood pressure and improve blood flow to the extremities. These medications can be used alone or in combination with other treatments, such as lifestyle modifications and alternative therapies, to manage Raynaud's disease and reduce cardiovascular risk. By dilating blood vessels and reducing blood pressure, these medications can help to improve blood flow to the extremities, reduce the frequency and severity of Raynaud's attacks, and lower the risk of cardiovascular complications.
Alternative Therapies to Enhance Cardiovascular Health
Alternative therapies can play a significant role in enhancing cardiovascular health, particularly for individuals with Raynaud's disease. Acupuncture, for instance, has been shown to improve blood flow and reduce inflammation, both of which can help alleviate symptoms of Raynaud's. Yoga and meditation can also be beneficial, as they can help reduce stress and promote relaxation, which can in turn help improve cardiovascular function. Herbal supplements such as ginkgo biloba and omega-3 fatty acids may also be helpful in improving blood flow and reducing inflammation. Additionally, biofeedback therapy can help individuals with Raynaud's disease learn to control their body's response to stress and cold temperatures, which can help reduce the frequency and severity of attacks. Furthermore, massage therapy can help improve blood flow and reduce muscle tension, which can also be beneficial for individuals with Raynaud's. By incorporating these alternative therapies into their treatment plan, individuals with Raynaud's disease may be able to reduce their cardiovascular risk and improve their overall health.