How Long Can You Keep Your Teeth With Periodontal Disease
Here is the introduction paragraph: Periodontal disease is a common oral health issue that affects millions of people worldwide, causing inflammation and infection of the gums and bone surrounding the teeth. If left untreated, periodontal disease can lead to tooth loss, which can have a significant impact on a person's quality of life. But how long can you keep your teeth with periodontal disease? The answer depends on several factors, including the severity of the disease, the effectiveness of treatment, and the individual's overall oral health. In this article, we will explore the relationship between periodontal disease and teeth longevity, discussing the impact of the disease on teeth, the factors that influence teeth longevity, and the ways to manage the disease to extend the life of your teeth. By understanding periodontal disease and its effects on teeth, you can take the first step towards preserving your smile. Understanding Periodontal Disease and Its Impact on Teeth Longevity is crucial in determining the longevity of your teeth.
Understanding Periodontal Disease and Its Impact on Teeth Longevity
Here is the introduction paragraph: Periodontal disease is a common and often misunderstood condition that affects millions of people worldwide. It is a chronic bacterial infection that targets the gums and bone supporting the teeth, leading to inflammation, damage, and potentially, tooth loss. But what exactly is periodontal disease, and how does it impact the longevity of our teeth? To understand this complex condition, it's essential to delve into the role of bacteria in its progression, the effects on the supporting structures of teeth, and the disease itself. By exploring these key aspects, we can gain a deeper understanding of periodontal disease and its far-reaching consequences. So, let's start by examining what periodontal disease is and how it affects teeth.
What is Periodontal Disease and How Does it Affect Teeth?
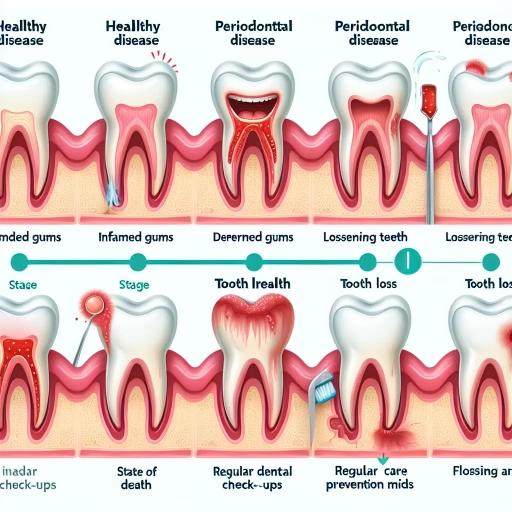
Periodontal disease, also known as gum disease, is a chronic bacterial infection that affects the gums and bone supporting the teeth. It occurs when plaque, a sticky film of bacteria, accumulates on the teeth and causes inflammation of the gums, leading to the destruction of the periodontal ligament and bone. If left untreated, periodontal disease can lead to the loss of teeth, as the supporting structures are compromised. The disease progresses through several stages, starting with gingivitis, a mild inflammation of the gums, to periodontitis, a more severe infection that can cause the gums to pull away from the teeth, creating pockets that trap bacteria and debris. Advanced periodontitis can lead to the loss of teeth, as the bone and periodontal ligament are severely damaged. Periodontal disease can also increase the risk of other health problems, such as heart disease, diabetes, and respiratory infections. Regular dental check-ups and good oral hygiene practices, such as brushing and flossing, can help prevent periodontal disease and detect it in its early stages, allowing for effective treatment and prevention of tooth loss.
The Role of Bacteria in Periodontal Disease Progression
The progression of periodontal disease is significantly influenced by the presence and activity of bacteria in the oral cavity. Periodontal pathogens, such as Porphyromonas gingivalis, Aggregatibacter actinomycetemcomitans, and Fusobacterium nucleatum, play a crucial role in the development and progression of the disease. These bacteria colonize the tooth surface and gingival crevice, producing virulence factors that trigger an inflammatory response in the host. The resulting inflammation leads to the destruction of the periodontal tissues, including the gingiva, periodontal ligament, and alveolar bone. As the disease progresses, the bacteria continue to thrive, forming complex biofilms that are resistant to the host's immune response and antimicrobial therapies. The biofilm's protective matrix allows the bacteria to persist and multiply, leading to further tissue damage and disease progression. Furthermore, the bacteria can also manipulate the host's immune response, suppressing the production of anti-inflammatory cytokines and promoting the production of pro-inflammatory cytokines, which exacerbates the disease. Therefore, understanding the role of bacteria in periodontal disease progression is essential for the development of effective therapeutic strategies to prevent and treat the disease.
How Periodontal Disease Affects the Supporting Structures of Teeth
Periodontal disease is a chronic bacterial infection that affects the supporting structures of teeth, including the periodontal ligament, cementum, and alveolar bone. As the disease progresses, it can cause inflammation and damage to these structures, leading to a loss of support for the teeth. The periodontal ligament, which connects the tooth to the surrounding bone, becomes inflamed and starts to break down, causing the tooth to become loose. The cementum, a thin layer of bone-like tissue that covers the root of the tooth, also becomes damaged, allowing bacteria to penetrate and cause further infection. The alveolar bone, which provides the foundation for the tooth, begins to resorb, or dissolve, leading to a decrease in the overall height of the bone and a loss of support for the tooth. As a result, teeth may become loose, shift, or even fall out. If left untreated, periodontal disease can lead to the loss of teeth and the need for costly and time-consuming dental restorations. Therefore, it is essential to seek professional dental care if symptoms of periodontal disease are present, such as bleeding gums, bad breath, or loose teeth, to prevent further damage and ensure the longevity of teeth.
Factors Influencing Teeth Longevity with Periodontal Disease
The longevity of teeth in individuals with periodontal disease is influenced by a multitude of factors. Disease severity, smoking and tobacco use, and genetics all play a significant role in determining the lifespan of teeth in those affected by this condition. The severity of periodontal disease can significantly impact the longevity of teeth, as more advanced stages of the disease can lead to increased tooth loss. Additionally, smoking and tobacco use have been shown to exacerbate periodontal disease, leading to a shorter lifespan for teeth. Furthermore, genetic predisposition can also affect the longevity of teeth, with some individuals being more susceptible to periodontal disease due to their genetic makeup. Understanding the impact of these factors is crucial in developing effective treatment plans and preventing tooth loss. The impact of disease severity on teeth longevity is a critical aspect of periodontal disease management, and it is essential to explore this topic further to determine the best course of treatment.
The Impact of Disease Severity on Teeth Longevity
The severity of periodontal disease has a significant impact on teeth longevity. As the disease progresses, the supporting structures of the teeth, including the periodontal ligament, bone, and gums, are damaged, leading to a decrease in teeth stability and an increase in the risk of tooth loss. In the early stages of periodontal disease, teeth may still be salvageable with proper treatment, and longevity can be extended. However, as the disease advances, the prognosis for teeth longevity becomes increasingly poor. Teeth with severe periodontal disease are more likely to be lost due to the extensive damage to the supporting structures, making it challenging to maintain them. Furthermore, the severity of periodontal disease can also affect the overall health of the surrounding teeth, leading to a higher risk of tooth loss and a decrease in overall teeth longevity. Therefore, it is essential to seek professional dental care to manage periodontal disease and prevent its progression to ensure the longest possible teeth longevity.
How Smoking and Tobacco Use Affect Teeth Longevity with Periodontal Disease
Smoking and tobacco use are significant risk factors for periodontal disease, which can severely impact teeth longevity. Tobacco use, in any form, damages the gums and bone that support the teeth, leading to periodontal disease. Smoking, in particular, reduces blood flow to the gums, making it harder for them to heal and increasing the risk of infection. This can cause the gums to pull away from the teeth, creating pockets that can trap bacteria and lead to further infection. As a result, smoking and tobacco use can accelerate the progression of periodontal disease, leading to tooth loss and reduced teeth longevity. In fact, studies have shown that smokers are up to four times more likely to develop periodontal disease than non-smokers, and are more likely to experience tooth loss. Furthermore, tobacco use can also reduce the effectiveness of periodontal treatments, making it harder to manage the disease and maintain healthy teeth. Quitting smoking and tobacco use is essential for maintaining healthy teeth and gums, and can significantly improve teeth longevity in individuals with periodontal disease.
The Role of Genetics in Determining Teeth Longevity with Periodontal Disease
The role of genetics in determining teeth longevity with periodontal disease is a significant factor that cannot be overlooked. Research has shown that genetic predisposition plays a crucial role in the development and progression of periodontal disease. Studies have identified several genetic variants that increase the risk of developing periodontal disease, including those that affect the immune system, inflammation, and tissue repair. For instance, genetic variations in the IL-1 gene cluster have been associated with an increased risk of aggressive periodontitis, a severe form of periodontal disease. Similarly, genetic variants in the MMP-1 gene have been linked to an increased risk of chronic periodontitis. Furthermore, genetic factors can also influence an individual's response to periodontal treatment, with some people being more responsive to therapy than others. A study published in the Journal of Periodontology found that individuals with a specific genetic variant in the VEGF gene had a better response to periodontal treatment than those without the variant. Overall, the role of genetics in determining teeth longevity with periodontal disease is complex and multifaceted, and further research is needed to fully understand the relationship between genetics and periodontal disease. However, it is clear that genetic factors can play a significant role in determining an individual's risk of developing periodontal disease and their response to treatment.
Managing Periodontal Disease to Extend Teeth Longevity
Managing periodontal disease is crucial to extend the longevity of teeth. Periodontal disease is a chronic bacterial infection that affects the gums and bone supporting the teeth, leading to inflammation, damage, and eventually tooth loss if left untreated. To manage periodontal disease effectively, it is essential to adopt a multi-faceted approach that includes regular dental check-ups and cleanings, scaling and root planing, and the use of antibiotics and other medications. Regular dental check-ups and cleanings play a vital role in preventing the progression of periodontal disease by removing plaque and tartar, identifying early signs of the disease, and providing personalized oral hygiene instructions. Scaling and root planing, on the other hand, help to remove plaque and tartar from below the gum line, reducing inflammation and preventing further damage. In some cases, antibiotics and other medications may be prescribed to help manage the disease. By incorporating these strategies into your oral care routine, you can effectively manage periodontal disease and extend the longevity of your teeth. Regular dental check-ups and cleanings are the first line of defense against periodontal disease, and it is essential to schedule regular appointments with your dentist to prevent the progression of the disease.
The Importance of Regular Dental Check-Ups and Cleanings
Regular dental check-ups and cleanings are crucial for maintaining good oral health and preventing the progression of periodontal disease. By visiting a dentist every six months, individuals can receive a thorough examination of their teeth and gums, allowing for the early detection of any potential issues. This includes the identification of plaque and tartar buildup, which can lead to inflammation and infection if left untreated. A professional cleaning, also known as a prophylaxis, removes these harmful substances, helping to prevent the development of periodontal disease and its associated complications. Furthermore, regular dental check-ups provide an opportunity for dentists to educate patients on proper oral hygiene techniques, such as brushing and flossing, and to recommend personalized treatment plans to address specific needs. By prioritizing regular dental check-ups and cleanings, individuals can significantly reduce their risk of developing periodontal disease and extend the longevity of their teeth.
How Scaling and Root Planing Can Help Manage Periodontal Disease
Scaling and root planing is a non-surgical procedure that can help manage periodontal disease by removing plaque, tartar, and bacteria from the teeth and roots. This procedure is usually performed by a dentist or periodontist and involves the use of specialized tools to remove the buildup of plaque and tartar, both above and below the gum line. By removing these deposits, scaling and root planing can help to reduce inflammation, prevent further damage to the gums and bone, and promote healing. Additionally, this procedure can help to smooth out the roots of the teeth, making it more difficult for bacteria to accumulate and cause further problems. Regular scaling and root planing can help to manage periodontal disease and prevent its progression, allowing individuals to maintain their natural teeth for a longer period. It is often recommended as a maintenance treatment for individuals with periodontal disease, and can be performed in conjunction with other treatments, such as antibiotics or surgical procedures, to help manage the disease. By incorporating scaling and root planing into their oral hygiene routine, individuals with periodontal disease can help to extend the life of their teeth and maintain a healthy, beautiful smile.
The Role of Antibiotics and Other Medications in Periodontal Disease Management
The management of periodontal disease often involves a combination of non-surgical and surgical treatments, with antibiotics and other medications playing a crucial role in controlling the infection and promoting healing. Antibiotics are typically prescribed to treat acute periodontal infections, such as abscesses, and to manage chronic periodontitis. The most commonly used antibiotics for periodontal disease are doxycycline, metronidazole, and amoxicillin, which target the bacteria that cause the infection. In addition to antibiotics, other medications such as anti-inflammatory agents, pain relievers, and antimicrobial mouthwashes may be prescribed to reduce inflammation, alleviate pain, and prevent the growth of bacteria. Furthermore, medications that target specific pathways involved in periodontal disease, such as matrix metalloproteinase inhibitors, are being researched and may offer new treatment options in the future. The use of antibiotics and other medications in periodontal disease management is often tailored to the individual patient's needs and may be used in conjunction with other treatments, such as scaling and root planing, to achieve optimal results. By controlling the infection and promoting healing, antibiotics and other medications can help to extend the longevity of teeth affected by periodontal disease.