How To Calculate Stroke Volume
Stroke volume, a crucial component of cardiac output, is a measure of the amount of blood pumped by the left ventricle of the heart in one contraction. Accurately calculating stroke volume is essential for healthcare professionals to assess cardiac function, diagnose cardiovascular diseases, and monitor the effectiveness of treatments. To grasp the concept of stroke volume, it is vital to understand its underlying principles, which will be discussed in the section "Understanding the Basics of Stroke Volume." Additionally, various methods can be employed to calculate stroke volume, including invasive and non-invasive techniques, which will be explored in "Calculating Stroke Volume Using Different Methods." Furthermore, the application of these calculations in clinical practice is crucial for making informed decisions about patient care, as discussed in "Applying the Calculations in Clinical Practice." By understanding the fundamentals of stroke volume and its calculation methods, healthcare professionals can provide better care for their patients. Therefore, let's start by understanding the basics of stroke volume.
Understanding the Basics of Stroke Volume
Stroke volume, a crucial component of cardiac function, plays a significant role in maintaining overall cardiovascular health. Understanding the basics of stroke volume is essential for healthcare professionals and individuals alike, as it can provide valuable insights into the heart's pumping efficiency. In this article, we will delve into the definition and importance of stroke volume, its normal ranges in adults and children, and the various factors that affect it, including heart rate and blood pressure. By grasping these fundamental concepts, readers will gain a deeper understanding of how stroke volume impacts cardiac function and overall well-being. To begin, let's explore the definition of stroke volume and its significance in maintaining optimal cardiac function.
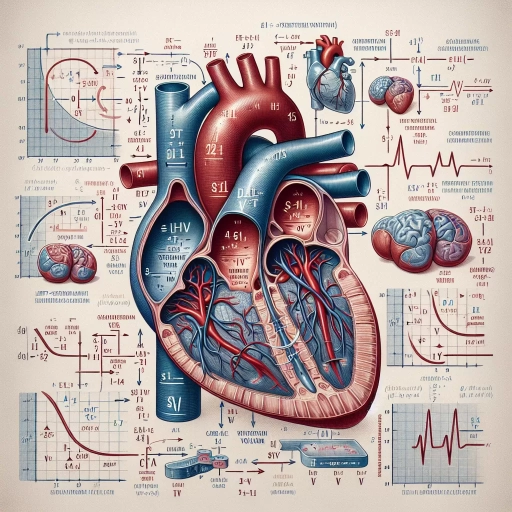
Definition of Stroke Volume and Its Importance in Cardiac Function
Stroke volume is defined as the volume of blood pumped by the left ventricle of the heart in a single beat. It is a crucial determinant of cardiac output, which is the total amount of blood pumped by the heart per minute. Stroke volume is calculated by subtracting the end-systolic volume from the end-diastolic volume of the left ventricle. The normal range for stroke volume in a healthy adult is between 60-120 mL. Maintaining optimal stroke volume is vital for ensuring adequate blood flow to meet the body's metabolic needs. A decrease in stroke volume can lead to decreased cardiac output, which can result in symptoms such as fatigue, shortness of breath, and decreased exercise tolerance. Conversely, an increase in stroke volume can lead to increased cardiac output, which is essential for meeting the increased metabolic demands during exercise or in response to stress. Factors such as preload, afterload, and contractility of the heart influence stroke volume, making it a complex and dynamic parameter. Understanding stroke volume and its importance in cardiac function is essential for diagnosing and managing cardiovascular diseases, such as heart failure, hypertension, and coronary artery disease. By monitoring and optimizing stroke volume, healthcare providers can improve patient outcomes and reduce the risk of cardiovascular complications.
Normal Ranges for Stroke Volume in Adults and Children
Stroke volume, a crucial parameter in cardiovascular physiology, refers to the amount of blood pumped by the left ventricle of the heart in one contraction. Normal ranges for stroke volume vary by age and physiological conditions. In adults, the typical stroke volume ranges from 60 to 130 milliliters (mL) per beat, with an average of around 80-100 mL. However, these values can fluctuate based on factors such as physical activity, posture, and overall health status. For instance, athletes or individuals who engage in regular exercise may have higher stroke volumes due to increased cardiac output demands. In contrast, individuals with heart failure or other cardiovascular conditions may exhibit lower stroke volumes. In children, stroke volume is generally lower due to their smaller heart size and lower blood volume. Newborns typically have a stroke volume of around 4-6 mL/kg, which increases to approximately 30-50 mL in toddlers and 50-80 mL in school-age children. As children grow and develop, their stroke volume continues to increase, eventually reaching adult values during adolescence. Understanding these normal ranges is essential for healthcare professionals to accurately diagnose and manage cardiovascular conditions, as well as for individuals to monitor their own cardiovascular health.
Factors Affecting Stroke Volume, Including Heart Rate and Blood Pressure
Stroke volume, the amount of blood pumped by the left ventricle of the heart in one contraction, is influenced by various factors, including heart rate and blood pressure. Heart rate, the number of heartbeats per minute, has an inverse relationship with stroke volume. As heart rate increases, stroke volume decreases, and vice versa. This is because the heart has less time to fill with blood between contractions at higher heart rates, resulting in a lower stroke volume. Conversely, at lower heart rates, the heart has more time to fill, allowing for a greater stroke volume. Blood pressure, specifically preload, also affects stroke volume. Preload refers to the initial stretching of the cardiac myocytes prior to contraction, and increased preload results in a greater stroke volume. This is because the heart is able to generate more force and pump more blood when it is stretched to a greater extent. Additionally, afterload, the pressure against which the heart must pump blood, also influences stroke volume. Increased afterload, such as in cases of hypertension, can decrease stroke volume as the heart must work harder to pump blood, resulting in a lower stroke volume. Other factors affecting stroke volume include contractility, the intrinsic ability of the heart to pump blood, and volume status, the amount of blood in the circulatory system. Understanding these factors is crucial in calculating stroke volume and diagnosing cardiovascular conditions.
Calculating Stroke Volume Using Different Methods
Calculating stroke volume is a crucial aspect of cardiovascular assessment, and there are several methods to achieve this. One of the most direct methods is the Fick principle, which involves measuring oxygen consumption and arterial-venous oxygen difference to calculate stroke volume. Another non-invasive method is echocardiography, which uses ultrasound waves to estimate stroke volume based on left ventricular dimensions and function. Additionally, pulse contour analysis is a minimally invasive method that uses arterial pressure waveform analysis to calculate stroke volume. Each of these methods has its own advantages and limitations, and understanding the principles behind them is essential for accurate calculation of stroke volume. The Fick principle, in particular, is considered the gold standard for measuring stroke volume, and it will be discussed in more detail below.
The Fick Principle: A Direct Method for Measuring Stroke Volume
The Fick principle is a direct method for measuring stroke volume, which is the amount of blood pumped by the heart with each beat. This principle was first described by Adolf Fick in 1870 and is based on the concept of oxygen consumption and cardiac output. The Fick principle states that the rate of oxygen consumption by the body is equal to the product of the cardiac output and the difference in oxygen content between arterial and venous blood. By measuring the oxygen consumption, cardiac output, and oxygen content of arterial and venous blood, stroke volume can be calculated using the Fick principle. This method is considered the gold standard for measuring stroke volume and is widely used in clinical and research settings. The Fick principle is particularly useful for measuring stroke volume in patients with heart failure, coronary artery disease, and other cardiovascular conditions. However, this method requires invasive procedures, such as cardiac catheterization, to measure oxygen content and cardiac output, which can be a limitation. Despite this, the Fick principle remains a valuable tool for accurately measuring stroke volume and understanding cardiovascular function.
Echocardiography: A Non-Invasive Method for Estimating Stroke Volume
Echocardiography is a non-invasive medical imaging technique that uses high-frequency sound waves to produce images of the heart and its blood vessels. In the context of estimating stroke volume, echocardiography is a valuable tool that provides a comprehensive assessment of cardiac function. By analyzing the images produced by echocardiography, healthcare professionals can measure the left ventricular end-diastolic volume (LVEDV) and left ventricular end-systolic volume (LVESV), which are essential parameters for calculating stroke volume. The technique involves the use of a transducer to transmit sound waves into the body, which are then reflected back to the transducer, creating a 2D or 3D image of the heart. Echocardiography can be performed in various modes, including M-mode, 2D, and Doppler, each providing unique information about cardiac structure and function. For stroke volume estimation, the most commonly used mode is the 2D mode, which allows for the measurement of left ventricular volumes and ejection fraction. Echocardiography is a widely accepted and reliable method for estimating stroke volume, and its non-invasive nature makes it an attractive option for patients who require repeated measurements or have contraindications for invasive procedures. Additionally, echocardiography can be performed at the bedside, making it a convenient and efficient tool for clinicians to assess cardiac function in a variety of settings. Overall, echocardiography is a valuable tool for estimating stroke volume, providing a non-invasive and accurate method for assessing cardiac function.
Pulse Contour Analysis: A Minimally Invasive Method for Calculating Stroke Volume
Pulse contour analysis is a minimally invasive method for calculating stroke volume, which involves analyzing the pulse waveform to estimate cardiac output. This technique uses a sensor placed on the patient's finger or wrist to measure the changes in blood pressure and flow with each heartbeat. The sensor detects the pulse waveform and sends the data to a monitor, which then uses algorithms to calculate stroke volume. Pulse contour analysis is based on the principle that the pulse waveform is directly related to the volume of blood ejected by the heart with each beat. By analyzing the shape and characteristics of the pulse waveform, the system can estimate the stroke volume with reasonable accuracy. This method is particularly useful in critically ill patients or those undergoing surgery, as it provides a continuous and real-time measurement of cardiac output without the need for invasive catheters. Additionally, pulse contour analysis can be used to monitor changes in stroke volume over time, allowing clinicians to adjust treatment strategies accordingly. Overall, pulse contour analysis is a valuable tool for calculating stroke volume and monitoring cardiac function in a variety of clinical settings.
Applying the Calculations in Clinical Practice
The application of hemodynamic calculations in clinical practice is crucial for healthcare professionals to make informed decisions about patient care. One key calculation is stroke volume, which can provide valuable insights into cardiac function. By applying stroke volume calculations, clinicians can assess cardiac function in patients with heart failure, monitor fluid therapy in critically ill patients, and interpret values in the context of other hemodynamic parameters. For instance, using stroke volume to assess cardiac function in patients with heart failure can help identify those at risk of decompensation, allowing for timely interventions. This calculation can also be used to monitor fluid therapy in critically ill patients, guiding the administration of fluids to optimize cardiac output. Furthermore, interpreting stroke volume values in the context of other hemodynamic parameters, such as cardiac output and systemic vascular resistance, can provide a more comprehensive understanding of a patient's cardiovascular status. By applying these calculations, clinicians can optimize patient care and improve outcomes. Using stroke volume to assess cardiac function in patients with heart failure is a critical application of this calculation, and it will be explored in more detail in the following section.
Using Stroke Volume to Assess Cardiac Function in Patients with Heart Failure
Stroke volume (SV) is a critical parameter in assessing cardiac function, particularly in patients with heart failure. It represents the amount of blood ejected by the left ventricle with each contraction, and its measurement can provide valuable insights into the heart's pumping efficiency. In patients with heart failure, a reduced stroke volume can indicate impaired cardiac function, which may be due to various factors such as decreased contractility, increased afterload, or ventricular remodeling. By using stroke volume to assess cardiac function, healthcare providers can identify patients who may benefit from targeted therapies, such as beta-blockers or ACE inhibitors, which can help improve cardiac function and reduce symptoms. Furthermore, stroke volume can be used to monitor the effectiveness of these therapies and adjust treatment plans accordingly. In addition, stroke volume can be used in conjunction with other hemodynamic parameters, such as cardiac output and systemic vascular resistance, to provide a more comprehensive understanding of cardiac function and guide clinical decision-making. Overall, the use of stroke volume to assess cardiac function in patients with heart failure is a valuable tool in the management of this complex and debilitating condition.
Monitoring Stroke Volume in Critically Ill Patients to Guide Fluid Therapy
Monitoring stroke volume in critically ill patients is crucial to guide fluid therapy, as it allows clinicians to optimize cardiac output and ensure adequate tissue perfusion. In critically ill patients, stroke volume can be affected by various factors such as cardiac dysfunction, hypovolemia, and vasopressor use. By continuously monitoring stroke volume, clinicians can identify patients who are at risk of developing cardiac dysfunction and adjust fluid therapy accordingly. For example, if a patient's stroke volume is decreasing despite adequate fluid resuscitation, it may indicate cardiac dysfunction, and the clinician may need to consider alternative treatments such as inotropes. On the other hand, if a patient's stroke volume is increasing with fluid therapy, it may indicate that the patient is responding well to treatment and further fluid administration may be warranted. Monitoring stroke volume can also help clinicians to avoid fluid overload, which is a common complication in critically ill patients. By tracking changes in stroke volume, clinicians can adjust fluid therapy to ensure that the patient is receiving the optimal amount of fluid to maintain adequate cardiac output without causing fluid overload. Overall, monitoring stroke volume is an essential component of fluid therapy in critically ill patients, and it can help clinicians to make informed decisions about fluid management and improve patient outcomes.
Interpreting Stroke Volume Values in the Context of Other Hemodynamic Parameters
Stroke volume (SV) is a critical component of cardiac output (CO), representing the volume of blood ejected by the left ventricle with each contraction. When interpreting SV values, it is essential to consider them in the context of other hemodynamic parameters to gain a comprehensive understanding of a patient's cardiovascular status. For instance, a low SV may be compensated by an elevated heart rate (HR), maintaining a normal CO. However, if the HR is also low, the resulting CO may be inadequate, leading to tissue hypoperfusion. Conversely, a high SV may be indicative of increased contractility, but if accompanied by elevated systemic vascular resistance (SVR), it may also suggest hypertension or cardiac hypertrophy. Furthermore, SV should be evaluated in conjunction with other parameters such as mean arterial pressure (MAP), pulmonary capillary wedge pressure (PCWP), and cardiac index (CI) to assess the overall cardiovascular performance. For example, a low SV with elevated PCWP may indicate left ventricular dysfunction, while a high SV with low PCWP may suggest volume overload. By considering SV in the context of these other hemodynamic parameters, clinicians can make more informed decisions regarding fluid management, vasopressor therapy, and inotropic support, ultimately optimizing patient outcomes.