What To Avoid When Taking Allopurinol
Allopurinol, a medication commonly prescribed to treat gout and high levels of uric acid, can be highly effective when used correctly. However, it is crucial to be aware of several key considerations to ensure safe and beneficial treatment. This article will delve into three critical areas that patients should be mindful of when taking allopurinol: common side effects to watch out for, interactions with other medications, and necessary lifestyle changes to avoid adverse effects. Understanding these factors can help mitigate potential risks and enhance the therapeutic benefits of the medication. By being informed about these aspects, patients can better manage their treatment plan and minimize the likelihood of complications. Let's start by examining the common side effects that patients should be vigilant about when taking allopurinol.
Common Side Effects to Watch Out For
When considering the potential side effects of various medications or treatments, it is crucial to be aware of several key areas that can impact your health. Common side effects can range from mild to severe and include potential allergic reactions, gastrointestinal issues, and changes in liver function. Allergic reactions can manifest in different ways, from mild skin rashes to life-threatening anaphylaxis, making it essential to monitor for any unusual symptoms. Gastrointestinal issues, such as nausea, vomiting, and diarrhea, can significantly affect daily life and may indicate a need for dosage adjustments or alternative treatments. Additionally, changes in liver function can be a silent but serious side effect, often requiring regular monitoring through blood tests. Understanding these potential side effects allows individuals to take proactive steps in managing their health and seeking medical advice when necessary. By being vigilant about these areas, individuals can better navigate the complexities of treatment and ensure their overall well-being. This article will delve into each of these critical areas, starting with **Potential Allergic Reactions**.
Potential Allergic Reactions
When taking allopurinol, it is crucial to be aware of potential allergic reactions, which can range from mild to severe. Allergic reactions to allopurinol are relatively rare but can be life-threatening if not recognized and treated promptly. One of the most significant allergic reactions is Stevens-Johnson syndrome (SJS), a rare but serious skin and mucous membrane disorder characterized by blistering and peeling of the skin, along with fever and other systemic symptoms. Another severe reaction is toxic epidermal necrolysis (TEN), which involves widespread skin necrosis and detachment. These conditions often require immediate medical attention and hospitalization. Milder allergic reactions may include skin rashes, hives, itching, and swelling, particularly of the face, lips, tongue, or throat. These symptoms can be uncomfortable but are generally less severe than SJS or TEN. However, any new rash or skin changes should be reported to a healthcare provider as soon as possible to determine if they are related to allopurinol use. In addition to skin manifestations, some individuals may experience respiratory symptoms such as wheezing, coughing, or shortness of breath due to an allergic reaction. Gastrointestinal symptoms like nausea, vomiting, or diarrhea can also occur. It is essential to monitor for these signs and seek medical advice if they persist or worsen over time. To mitigate the risk of allergic reactions, it is recommended that patients start with a low dose of allopurinol and gradually increase it under the supervision of a healthcare provider. Regular follow-up appointments can help in early detection of any adverse effects. Patients should also be educated on what constitutes an emergency and when to seek immediate medical help. In cases where an allergic reaction is suspected, discontinuing allopurinol and consulting a healthcare provider promptly is crucial. Alternative treatments may be necessary to manage the underlying condition for which allopurinol was prescribed, such as gout or high levels of uric acid. By being vigilant about potential allergic reactions and taking proactive steps, individuals can minimize risks associated with allopurinol therapy and ensure safe and effective treatment.
Gastrointestinal Issues
When taking allopurinol, it is crucial to be aware of potential gastrointestinal issues that may arise as common side effects. Gastrointestinal problems can range from mild discomfort to severe complications, making it essential to monitor your body's response closely. One of the most frequent gastrointestinal side effects is nausea, which can sometimes escalate to vomiting. This can be particularly problematic as it may lead to dehydration and electrolyte imbalances if not managed properly. Additionally, patients may experience abdominal pain or cramping, which can vary in intensity and may be accompanied by bloating or gas. Diarrhea or constipation are also possible, disrupting normal bowel habits and potentially causing further discomfort. In some cases, more severe gastrointestinal issues such as gastritis or ulcers may develop, necessitating immediate medical attention. It is important to note that these side effects can often be mitigated by taking allopurinol with food or adjusting the dosage under the guidance of a healthcare provider. If you notice any persistent or severe gastrointestinal symptoms, it is vital to consult your doctor promptly to avoid any long-term damage and ensure the safe continuation of your treatment. Early recognition and management of these side effects can significantly improve your overall health and well-being while on allopurinol therapy.
Liver Function Changes
When taking allopurinol, it is crucial to monitor liver function closely, as changes in liver health can be a significant side effect. Allopurinol, a medication used to treat gout and high levels of uric acid, can sometimes cause liver damage or elevate liver enzymes. This is because the drug is metabolized by the liver, and in some individuals, it may trigger an adverse reaction. If you experience symptoms such as jaundice (yellowing of the skin and eyes), dark urine, pale stools, or severe abdominal pain, these could be indicative of liver dysfunction. Additionally, fatigue, loss of appetite, or nausea may also signal liver issues. Regular blood tests to check liver enzyme levels are essential while on allopurinol to detect any abnormalities early. If your healthcare provider notices elevated liver enzymes or other signs of liver damage, they may adjust your dosage or switch you to a different medication. It is vital to report any unusual symptoms promptly to prevent further complications. Monitoring liver function not only ensures the safe use of allopurinol but also helps in maintaining overall health and preventing potential long-term damage to this critical organ. By being vigilant about these changes and communicating openly with your healthcare provider, you can mitigate the risk of severe side effects and continue managing your condition effectively.
Interactions with Other Medications
Interactions between medications can have significant impacts on patient health, making it crucial to understand how different drugs interact with each other. This article delves into the complexities of these interactions, focusing on three critical areas: anticoagulants and blood thinners, diuretics and blood pressure medications, and chemotherapy drugs. Each of these categories presents unique challenges and potential risks that healthcare providers must consider to ensure safe and effective treatment. For instance, anticoagulants and blood thinners can increase the risk of bleeding when combined with other medications, while diuretics and blood pressure medications can lead to adverse effects such as hypotension or electrolyte imbalances. Chemotherapy drugs, known for their potent effects, can interact with a wide range of medications, altering their efficacy or toxicity. Understanding these interactions is essential for preventing adverse reactions and optimizing patient outcomes. This article will explore these topics in detail, starting with the critical interactions involving anticoagulants and blood thinners.
Anticoagulants and Blood Thinners
When considering the interactions of allopurinol with other medications, it is crucial to understand the implications of combining it with anticoagulants and blood thinners. Anticoagulants and blood thinners are medications designed to prevent blood clots from forming or growing. These include warfarin, heparin, aspirin, and newer oral anticoagulants like rivaroxaban and apixaban. When taken alongside allopurinol, which is used to treat gout and high levels of uric acid, there can be significant interactions that necessitate careful monitoring. Allopurinol can enhance the anticoagulant effect of warfarin, leading to an increased risk of bleeding. This is because allopurinol inhibits the metabolism of warfarin, causing higher levels of the anticoagulant in the bloodstream. As a result, patients on both medications may require more frequent monitoring of their international normalized ratio (INR) to adjust warfarin dosages accordingly. Similarly, combining allopurinol with other blood thinners such as aspirin or clopidogrel can also increase the risk of bleeding due to additive effects on platelet function and coagulation pathways. Moreover, the concomitant use of allopurinol with newer oral anticoagulants like rivaroxaban or apixaban may not have as well-documented interactions as with warfarin, but caution is still advised. These medications work through different mechanisms but still carry a risk of increased bleeding when combined with other drugs that affect coagulation. To manage these interactions effectively, healthcare providers often recommend regular monitoring of patients' coagulation status and adjustment of medication dosages as needed. Patients should be educated on the signs of bleeding and encouraged to report any unusual symptoms promptly. Additionally, alternative treatments for gout or hyperuricemia might be considered if the risk of bleeding is deemed too high. In summary, the combination of allopurinol with anticoagulants and blood thinners requires careful management to mitigate the risk of adverse interactions. Regular monitoring and dose adjustments are essential to ensure patient safety while maintaining therapeutic efficacy.
Diuretics and Blood Pressure Medications
When considering the interactions between allopurinol and other medications, it is crucial to understand the potential effects of diuretics and blood pressure medications. Diuretics, which are used to treat conditions like hypertension and edema by increasing urine production, can interact with allopurinol in several ways. For instance, thiazide diuretics can increase the risk of allopurinol-induced hypersensitivity reactions, such as severe skin rashes or even life-threatening conditions like Stevens-Johnson syndrome. This is because thiazides can elevate serum uric acid levels, which may exacerbate the side effects associated with allopurinol. Blood pressure medications, particularly those in the class of ACE inhibitors (angiotensin-converting enzyme inhibitors) and beta-blockers, also require careful consideration when taken alongside allopurinol. ACE inhibitors, which lower blood pressure by relaxing blood vessels, can increase the levels of allopurinol in the body due to their effect on renal function. This heightened concentration of allopurinol may enhance its therapeutic effects but also increases the risk of adverse reactions such as gastrointestinal disturbances, liver enzyme elevations, and hypersensitivity reactions. Beta-blockers, another common class of blood pressure medications that reduce heart rate and blood pressure, may interact with allopurinol by affecting its metabolism. Some beta-blockers can alter the activity of enzymes involved in the metabolism of allopurinol, leading to higher plasma concentrations and potentially increasing the risk of side effects. Additionally, loop diuretics like furosemide can affect kidney function and alter the excretion of allopurinol, potentially leading to higher serum levels and increased toxicity. It is essential for patients taking allopurinol to closely monitor their kidney function and adjust dosages accordingly when using these diuretics. In summary, when taking allopurinol, it is vital to be aware of the potential interactions with diuretics and blood pressure medications. These interactions can significantly impact both the efficacy and safety profile of allopurinol treatment. Patients should consult their healthcare providers to manage these interactions effectively and minimize the risk of adverse effects. Regular monitoring of kidney function, liver enzymes, and serum uric acid levels is recommended to ensure safe co-administration of these medications. By understanding these interactions, healthcare providers can tailor treatment plans to optimize therapeutic outcomes while minimizing risks.
Chemotherapy Drugs
Chemotherapy drugs are potent medications designed to target and destroy rapidly dividing cancer cells. However, their interaction with other medications, including allopurinol, can be complex and potentially hazardous. When taking allopurinol, a drug used to treat gout and high levels of uric acid, it is crucial to be aware of these interactions to avoid adverse effects. Chemotherapy agents can induce a rapid breakdown of cancer cells, leading to the release of large amounts of uric acid into the bloodstream—a condition known as tumor lysis syndrome. Allopurinol is often prescribed to prevent this syndrome by inhibiting the enzyme xanthine oxidase, which is involved in uric acid production. However, combining allopurinol with certain chemotherapy drugs can enhance the risk of adverse reactions. For instance, some chemotherapy agents like cyclophosphamide and doxorubicin can increase the toxicity of allopurinol, leading to severe side effects such as bone marrow suppression and liver damage. Moreover, allopurinol can interact with other medications that are commonly used in conjunction with chemotherapy, such as mercaptopurine and azathioprine. These interactions can significantly alter the metabolism and efficacy of these drugs, potentially reducing their therapeutic effects or increasing their toxicity. For example, allopurinol can inhibit the metabolism of mercaptopurine, leading to elevated levels of this drug in the body and increasing the risk of myelosuppression—a condition characterized by decreased production of blood cells. Given these potential interactions, it is essential for patients undergoing chemotherapy to closely monitor their medication regimen and report any changes or additions to their healthcare provider. Regular monitoring of blood counts, liver function tests, and uric acid levels can help mitigate the risks associated with these interactions. Additionally, adjusting the dosage of either allopurinol or the chemotherapy agent may be necessary to minimize adverse effects while maintaining therapeutic efficacy. In summary, the interaction between chemotherapy drugs and allopurinol necessitates careful management to prevent serious complications. By understanding these interactions and taking appropriate precautions, patients can reduce the risk of adverse reactions and ensure safe and effective treatment outcomes.
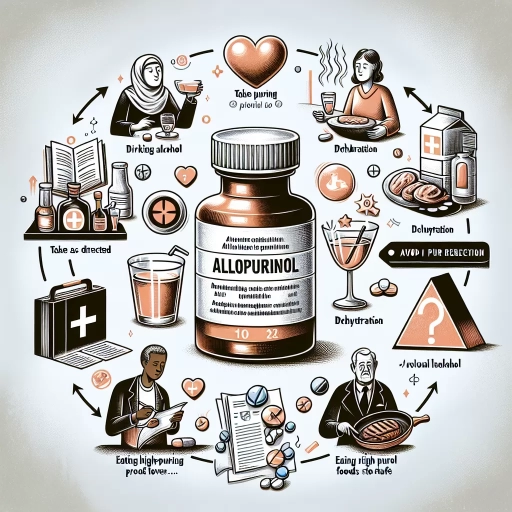
Lifestyle Changes to Avoid Adverse Effects
Lifestyle changes are crucial in avoiding adverse health effects, and understanding the key areas to focus on can significantly improve overall well-being. Three critical lifestyle adjustments include reducing excessive alcohol consumption, limiting high-purine foods and drinks, and ensuring adequate hydration. Excessive alcohol consumption can lead to a myriad of health issues, including liver damage, cardiovascular problems, and increased risk of certain cancers. High-purine foods and drinks, such as red meat and seafood, can exacerbate conditions like gout and kidney stones. Dehydration, on the other hand, can impair cognitive function, reduce physical performance, and lead to severe health complications if left unaddressed. By making informed choices in these areas, individuals can mitigate these risks and maintain a healthier lifestyle. Starting with one of the most immediate and impactful changes, reducing excessive alcohol consumption is a vital step towards better health. This adjustment not only helps in preventing chronic diseases but also improves mental clarity and overall quality of life. Therefore, understanding the implications of excessive alcohol consumption is essential for initiating a healthier lifestyle journey.
Excessive Alcohol Consumption
Excessive alcohol consumption is a significant lifestyle factor that can exacerbate the adverse effects of allopurinol, a medication commonly prescribed to treat gout and high levels of uric acid. Alcohol not only increases uric acid production but also impairs the body's ability to eliminate it, leading to higher uric acid levels and potentially worsening gout symptoms. Furthermore, alcohol can strain the liver, which is already working to metabolize allopurinol. This dual burden on the liver can lead to increased toxicity and reduced efficacy of the medication. Additionally, excessive alcohol intake can lead to dehydration, which may enhance the risk of kidney stones—a known side effect of allopurinol. The combination of alcohol and allopurinol can also heighten the risk of gastrointestinal issues such as nausea, vomiting, and diarrhea. To avoid these adverse effects, it is crucial to limit or avoid alcohol consumption entirely while taking allopurinol. By making this lifestyle change, individuals can better manage their gout symptoms, reduce the risk of medication side effects, and maintain overall health and well-being. This proactive approach ensures that the therapeutic benefits of allopurinol are maximized without compromising patient safety.
High-Purine Foods and Drinks
When taking allopurinol, it is crucial to be mindful of high-purine foods and drinks to avoid adverse effects. High-purine foods are those that contain a significant amount of purines, which the body converts into uric acid. Elevated uric acid levels can exacerbate conditions like gout, making it essential to manage dietary intake. Foods with high purine content include organ meats such as liver, kidney, and sweetbreads; seafood like anchovies, sardines, mussels, and scallops; and certain types of fish like herring and mackerel. Meat products such as bacon, sausage, and ham are also high in purines. Additionally, some vegetables like asparagus, mushrooms, and spinach contain moderate to high levels of purines. Beverages can also contribute to purine intake; beer and wine are particularly high in purines. Even some soft drinks and sugary beverages can indirectly increase uric acid levels due to their high sugar content. To mitigate these effects while on allopurinol, it is advisable to adopt a balanced diet that limits or avoids these high-purine foods and drinks. Instead, focus on consuming low-purine foods such as dairy products, eggs, nuts, and most fruits and vegetables. Drinking plenty of water is also recommended to help flush out uric acid from the body. By making these lifestyle changes and being aware of the dietary sources of purines, individuals can better manage their condition and minimize the risk of adverse effects associated with allopurinol treatment. This proactive approach not only helps in maintaining optimal health but also enhances the efficacy of the medication. In summary, understanding and managing high-purine foods and drinks is a key component of lifestyle changes necessary to avoid adverse effects when taking allopurinol. By choosing a diet rich in low-purine foods and limiting or avoiding high-purine items, individuals can significantly improve their health outcomes and ensure the medication works effectively.
Dehydration and Inadequate Hydration
Dehydration and inadequate hydration are critical health concerns that can significantly impact overall well-being, particularly for individuals taking medications like allopurinol. Allopurinol, commonly prescribed to manage gout and high levels of uric acid, requires adequate hydration to function effectively and minimize potential side effects. When the body is dehydrated, it cannot efficiently process and eliminate the medication, leading to increased risks of adverse reactions such as kidney stones, liver damage, and severe skin reactions. Inadequate hydration can also exacerbate gout symptoms, creating a vicious cycle where the condition worsens due to insufficient fluid intake. Drinking plenty of water helps to dilute uric acid in the blood and urine, facilitating its excretion and reducing the likelihood of kidney stone formation. Furthermore, proper hydration supports liver function, which is essential for metabolizing allopurinol. By maintaining optimal fluid levels, individuals can enhance the efficacy of their medication while mitigating potential side effects. Therefore, it is imperative to prioritize hydration as a lifestyle change when taking allopurinol to avoid adverse effects and ensure the best possible outcomes in managing gout and related conditions. Regularly monitoring urine output and color can serve as a simple yet effective indicator of hydration status; if urine is dark yellow or output is low, it may signal the need for increased fluid intake. Incorporating hydrating foods like watermelon, cucumbers, and celery into one's diet can also contribute to maintaining adequate hydration levels. By adopting these simple yet crucial lifestyle changes, individuals can significantly reduce the risk of dehydration-related complications associated with allopurinol treatment.