What Is Perineum Pain In Females
Perineum pain in females is a significant health concern that affects many women, often going unaddressed due to stigma or lack of awareness. The perineum, the area between the vagina and anus, is a sensitive region that can experience discomfort for various reasons. Understanding the nature of perineum pain is crucial for effective management and treatment. This article delves into the complexities of perineum pain, starting with an in-depth exploration of **Understanding Perineum Pain in Females**, where we will discuss the anatomy and common symptoms associated with this condition. We will then examine **Causes and Risk Factors of Perineum Pain**, highlighting the various medical, lifestyle, and environmental factors that contribute to its development. Finally, we will provide insights into **Diagnosis, Treatment, and Management of Perineum Pain**, outlining the diagnostic processes and treatment options available to alleviate this discomfort. By understanding these aspects, women can better navigate their health and seek appropriate care when needed. Let's begin by **Understanding Perineum Pain in Females**.
Understanding Perineum Pain in Females
Perineum pain in females is a common yet often misunderstood condition that can significantly impact daily life. To fully comprehend this issue, it is essential to delve into several key aspects. First, understanding the **definition and location of the perineum** is crucial, as this area plays a vital role in both anatomical and functional terms. Knowing where the perineum is situated and its role in the body sets the foundation for further exploration. Second, identifying the **common causes of perineum pain** helps in diagnosing and treating the condition effectively. These causes can range from childbirth and pelvic floor disorders to infections and trauma. Lastly, **distinguishing perineum pain from other pelvic pains** is vital to ensure accurate diagnosis and appropriate treatment, as symptoms can sometimes overlap with other conditions such as vulvodynia or endometriosis. By examining these facets, individuals can gain a comprehensive understanding of perineum pain and seek the right medical advice. Let's begin by exploring the **definition and location of the perineum**, which serves as the cornerstone for understanding this complex issue.
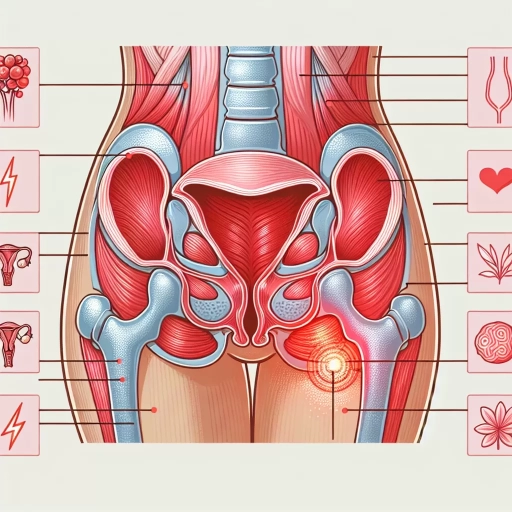
Definition and Location of the Perineum
The perineum is a complex anatomical region located between the pubic symphysis (the front of the pelvis) and the coccyx (tailbone), extending from the base of the penis or clitoris to the anus. In females, it is situated between the vulva and the anus, encompassing the external genitalia and surrounding tissues. This area is divided into two parts: the urogenital triangle, which contains the urethra and vagina, and the anal triangle, which surrounds the anus. The perineum plays a crucial role in supporting pelvic organs, facilitating childbirth, and aiding in the control of urination and defecation. Its rich network of nerves, blood vessels, and muscles makes it highly sensitive and prone to injury or strain, particularly during childbirth or physical activities. Understanding the precise location and function of the perineum is essential for diagnosing and managing perineum pain in females, which can arise from various causes including childbirth trauma, infections, or chronic conditions such as vulvodynia or pelvic floor dysfunction. Recognizing the anatomy of this region helps healthcare providers and individuals alike to address symptoms effectively and maintain overall pelvic health.
Common Causes of Perineum Pain
Perineum pain in females can arise from a variety of causes, each with distinct underlying factors. One common cause is childbirth, particularly if the perineum was severely stretched or torn during delivery. This trauma can lead to chronic pain and discomfort, often exacerbated by activities such as sitting or walking. Another significant cause is pelvic floor dysfunction, where the muscles in the pelvic floor become weak or tight, leading to pain and discomfort in the perineal area. Infections like urinary tract infections (UTIs) or vaginal infections can also cause perineum pain due to inflammation and irritation. Additionally, conditions such as vulvodynia, characterized by chronic pain in the vulva, can extend to the perineum. Gynecological procedures like episiotomies or surgical repairs can sometimes result in persistent pain if not properly healed. Furthermore, certain medical conditions such as endometriosis, where tissue similar to the lining of the uterus grows outside the uterus, can cause perineal pain due to the proximity of affected areas. Lifestyle factors such as prolonged sitting, tight clothing, or poor hygiene practices can also contribute to perineum pain. Lastly, psychological factors like stress and anxiety can exacerbate physical discomfort, making it essential to address both physical and mental health aspects when managing perineum pain. Understanding these causes is crucial for effective diagnosis and treatment, ensuring that women receive appropriate care to alleviate their symptoms and improve their quality of life.
Distinguishing Perineum Pain from Other Pelvic Pains
Distinguishing perineum pain from other pelvic pains is crucial for accurate diagnosis and effective treatment. The perineum, the area between the vagina and anus, can experience pain due to various reasons such as childbirth, trauma, or infections. To differentiate it from other pelvic pains, it's essential to consider the location and nature of the pain. Perineum pain is typically localized to the perineal region and may be described as sharp, stabbing, or aching. In contrast, pelvic pain can be more diffuse and may radiate to the lower abdomen, back, or thighs. Key distinguishing factors include the timing and triggers of the pain. For instance, perineum pain often worsens with activities that put pressure on the area, such as sitting or straining during bowel movements. On the other hand, pelvic pain might be exacerbated by menstrual cycles, sexual activity, or certain movements. Additionally, perineum pain is often associated with specific conditions like episiotomy scars, perineal tears, or vulvodynia, whereas pelvic pain could be linked to broader issues like endometriosis, ovarian cysts, or urinary tract infections. A thorough medical history and physical examination are vital for distinguishing between these types of pain. Healthcare providers may perform a pelvic exam to assess for tenderness in the perineal area and look for signs of infection or trauma. Imaging tests like ultrasound or MRI might also be used to rule out other pelvic conditions. Understanding the specific characteristics of perineum pain helps in tailoring treatment approaches, which could include physical therapy, pain management medications, or surgical interventions if necessary. In summary, distinguishing perineum pain from other pelvic pains requires careful consideration of the pain's location, nature, timing, and triggers. Accurate diagnosis through comprehensive medical evaluation is essential for providing appropriate treatment and alleviating symptoms effectively.
Causes and Risk Factors of Perineum Pain
Perineum pain, a condition affecting the area between the anus and the vulva in women or the scrotum in men, can arise from a variety of causes and risk factors. Understanding these underlying factors is crucial for effective diagnosis and treatment. This article delves into three primary areas that contribute to perineum pain: childbirth and perineal trauma, medical conditions and infections, and lifestyle factors and physical activities. Childbirth, particularly if it involves significant perineal trauma such as episiotomies or severe tears, can lead to chronic pain in the perineal region. Medical conditions like infections, abscesses, or inflammatory diseases also play a significant role in causing discomfort. Additionally, lifestyle factors such as prolonged sitting, certain physical activities, and poor hygiene practices can exacerbate the issue. By examining these distinct yet interconnected causes, individuals can better comprehend their risk factors and seek appropriate medical attention. Let's begin by exploring how childbirth and perineal trauma contribute to perineum pain.
Childbirth and Perineal Trauma
Childbirth is a significant life event that can have various physical impacts on women, one of which is perineal trauma. Perineal trauma refers to injuries that occur to the perineum, the area between the vagina and anus, during childbirth. These injuries can range from minor tears to more severe lacerations and episiotomies (surgical incisions made to widen the vaginal opening). The causes and risk factors for perineal trauma are multifaceted. One primary factor is the size and position of the baby; larger babies or those in certain positions, such as posterior presentation, increase the likelihood of perineal injury. Additionally, first-time mothers are at higher risk due to less elasticity in their perineal tissues compared to women who have given birth before. The use of instruments like forceps or vacuum extractors during delivery also elevates the risk of severe perineal trauma. Other contributing factors include prolonged second stage of labor, epidural anesthesia which can reduce the mother's ability to feel and push effectively, and previous history of perineal trauma. Furthermore, certain maternal characteristics such as younger age and higher body mass index (BMI) can also increase the risk. Understanding these causes and risk factors is crucial for healthcare providers to implement preventive measures and appropriate management strategies to minimize the occurrence and severity of perineal trauma during childbirth. This includes techniques like perineal massage during pregnancy, controlled pushing during labor, and careful suturing post-delivery to promote healing and reduce long-term complications such as chronic pain and incontinence. By acknowledging these factors, healthcare providers can better support women in reducing their risk of perineal trauma and ensuring a smoother recovery post-childbirth.
Medical Conditions and Infections
Perineum pain in females can be attributed to a variety of medical conditions and infections, each with its own set of causes and risk factors. One common cause is **vaginal infections**, such as bacterial vaginosis or yeast infections, which can lead to inflammation and discomfort in the perineal area. **Urinary Tract Infections (UTIs)** are another significant contributor, as they can cause pain and irritation that radiates to the perineum. **Sexually Transmitted Infections (STIs)** like herpes simplex virus or chlamydia can also result in perineal pain due to the inflammation and lesions they cause. **Pelvic inflammatory disease (PID)**, which involves infection of the female reproductive organs, is another potential cause. PID can lead to chronic pelvic pain that includes the perineal region. **Endometriosis**, a condition where tissue similar to the lining of the uterus grows outside the uterus, can cause severe pelvic and perineal pain, especially during menstruation. **Hemorrhoids** and **anal fissures** are additional conditions that can cause perineal pain due to the discomfort and inflammation they produce. **Childbirth-related injuries**, such as episiotomies or severe tears during delivery, can lead to long-term perineal pain. **Vulvodynia**, a condition characterized by chronic pain in the vulva, can also extend to the perineal area. **Inflammatory bowel diseases** like Crohn's disease or ulcerative colitis may cause perineal pain due to fistulas or abscesses that form in the rectal area. Understanding these underlying medical conditions and infections is crucial for diagnosing and treating perineum pain effectively in females. Each condition has its own risk factors, such as sexual activity, hygiene practices, and previous medical history, which healthcare providers must consider when evaluating patients. Accurate diagnosis and appropriate treatment can significantly alleviate perineum pain and improve quality of life for affected women.
Lifestyle Factors and Physical Activities
Lifestyle factors and physical activities play a significant role in the development and management of perineum pain in females. Sedentary lifestyles, for instance, can contribute to weakened pelvic floor muscles, which are crucial for supporting the perineal region. Conversely, regular physical activity, such as walking, swimming, or cycling, can help strengthen these muscles and improve overall pelvic health. However, certain activities may exacerbate perineum pain; for example, high-impact sports like running or jumping can increase pressure on the perineum, especially if proper supportive gear is not used. Additionally, poor posture during daily activities or exercise can strain the muscles and ligaments in the perineal area, leading to discomfort. Proper body mechanics and ergonomic practices are essential to avoid unnecessary strain. Lifestyle choices such as smoking and obesity also impact perineum health negatively; smoking reduces blood flow and oxygen delivery to tissues, while obesity increases pressure on the pelvic floor. Furthermore, dietary habits that lead to constipation or straining during bowel movements can cause significant stress on the perineal area. A balanced diet rich in fiber and adequate hydration helps prevent constipation and reduces the risk of perineum pain. Stress management techniques like yoga or meditation can also help alleviate muscle tension that may contribute to perineal discomfort. In summary, adopting a healthy lifestyle that includes regular physical activity, maintaining a healthy weight, avoiding harmful habits like smoking, and practicing good body mechanics are all critical in preventing and managing perineum pain in females.
Diagnosis, Treatment, and Management of Perineum Pain
Perineum pain, a condition affecting the area between the pubic symphysis and the coccyx, can significantly impact an individual's quality of life. Diagnosing and managing this pain requires a comprehensive approach that includes various diagnostic procedures, medical treatments, and lifestyle adjustments. To accurately identify the cause of perineum pain, healthcare providers must employ specific diagnostic procedures and tests. These may include physical examinations, imaging studies such as MRI or ultrasound, and sometimes biopsies to rule out underlying conditions like infections or tumors. Once a diagnosis is made, medical treatments and therapies can be tailored to address the specific cause of the pain. These treatments may involve medications, physical therapy, or in some cases, surgical interventions. Additionally, lifestyle changes and self-care strategies play a crucial role in managing perineum pain. These can include dietary modifications, pelvic floor exercises, and stress management techniques. By understanding these three key components—diagnostic procedures and tests, medical treatments and therapies, and lifestyle changes and self-care strategies—individuals can better navigate the process of alleviating perineum pain. Let's begin by exploring the essential diagnostic procedures and tests that lay the foundation for effective treatment.
Diagnostic Procedures and Tests
Diagnostic procedures and tests play a crucial role in accurately identifying the underlying causes of perineum pain in females. To begin with, a thorough medical history and physical examination are essential. The healthcare provider will ask detailed questions about the nature of the pain, its duration, and any factors that exacerbate or alleviate it. A pelvic examination may be performed to assess for any abnormalities or tenderness in the perineal area. Imaging tests such as ultrasound, MRI (Magnetic Resonance Imaging), or CT (Computed Tomography) scans can help identify structural issues like cysts, tumors, or other anatomical abnormalities that could be contributing to the pain. For instance, an ultrasound can detect conditions such as Bartholin's cysts or abscesses, while an MRI can provide detailed images of soft tissues and help diagnose conditions like endometriosis or pelvic floor dysfunction. Laboratory tests may also be ordered to rule out infections. A urinalysis can check for urinary tract infections (UTIs), and blood tests can help identify inflammatory markers or hormonal imbalances. Additionally, swabs may be taken from the vaginal or perineal area to test for sexually transmitted infections (STIs) such as herpes simplex virus or chlamydia. Specialized tests like electromyography (EMG) of the pelvic floor muscles can assess muscle function and identify any muscle spasms or weakness that could be contributing to pain. Similarly, urodynamic studies may be conducted if there are symptoms suggesting urinary incontinence or other bladder issues. In some cases, a diagnostic laparoscopy might be recommended to visually inspect the pelvic organs for conditions like endometriosis or adhesions. This minimally invasive procedure involves inserting a small camera through an incision in the abdomen to view the internal organs. Lastly, psychological evaluations may also be part of the diagnostic process since chronic pain can have a significant psychological component. Assessing mental health through questionnaires and interviews helps in understanding any underlying stressors or coping mechanisms that might influence pain perception. By combining these diagnostic tools, healthcare providers can accurately diagnose the cause of perineum pain in females and develop an effective treatment plan tailored to the individual's needs.
Medical Treatments and Therapies
Medical treatments and therapies for perineum pain in females are multifaceted and tailored to address the underlying causes of the discomfort. **Physical Therapy** plays a crucial role, focusing on pelvic floor exercises such as Kegel exercises to strengthen the muscles and improve bladder control. Physical therapists may also employ techniques like biofeedback, electrical stimulation, and manual therapy to relax tense muscles and improve blood flow to the area. **Pain Management** strategies include the use of analgesics, anti-inflammatory medications, and in some cases, nerve blocks or injections to alleviate severe pain. **Topical Treatments** such as creams or ointments containing lidocaine or capsaicin can be applied directly to the perineal area to reduce pain and discomfort. **Behavioral Therapies** are also effective, particularly cognitive-behavioral therapy (CBT), which helps patients manage pain by changing their perception and response to it. **Relaxation Techniques** like deep breathing, progressive muscle relaxation, and mindfulness meditation can reduce stress and alleviate pain. For women experiencing perineum pain due to conditions like vulvodynia or vaginismus, **Sex Therapy** may be recommended to address any psychological or emotional factors contributing to the pain. In cases where the pain is associated with infections or inflammatory conditions, **Antibiotics** or **Anti-inflammatory Medications** may be prescribed. For chronic conditions such as endometriosis or interstitial cystitis, **Hormonal Therapies** or **Immunosuppressive Drugs** might be necessary. **Surgical Interventions** are considered in severe cases where other treatments have failed; procedures such as perineoplasty or nerve decompression surgery may be performed. **Alternative Therapies** like acupuncture and herbal remedies are also explored by some patients, although their efficacy varies and more research is needed to fully understand their benefits. **Lifestyle Modifications**, including dietary changes, regular exercise, and avoiding irritants that exacerbate the condition, are crucial in managing perineum pain effectively. By combining these medical treatments and therapies, healthcare providers can offer comprehensive care that addresses both the physical and emotional aspects of perineum pain in females.
Lifestyle Changes and Self-Care Strategies
Lifestyle changes and self-care strategies play a crucial role in managing perineum pain in females, complementing medical diagnosis, treatment, and management. To alleviate discomfort, it is essential to adopt a holistic approach that includes dietary adjustments, physical activity modifications, and stress reduction techniques. Starting with diet, incorporating foods rich in omega-3 fatty acids, antioxidants, and fiber can help reduce inflammation and improve overall pelvic health. Avoiding spicy or acidic foods that may irritate the perineal area is also advisable. Regular physical activity, such as gentle exercises like yoga or swimming, can enhance blood circulation and strengthen pelvic muscles without exacerbating pain. However, it is important to avoid high-impact activities that may put additional strain on the perineum. Proper hygiene practices are also vital; using mild soaps and avoiding harsh chemicals can prevent irritation. Wearing loose, breathable clothing can reduce friction and discomfort. For women experiencing perineum pain during menstruation, using heating pads or warm compresses can provide relief by relaxing the muscles and improving blood flow. Engaging in stress-reducing activities such as meditation, deep breathing exercises, or mindfulness can help manage pain by reducing overall stress levels. Additionally, maintaining a healthy weight through balanced eating and regular exercise can reduce pressure on the perineal area. Avoiding prolonged sitting or standing and taking regular breaks to stretch can also help alleviate discomfort. For women who experience pain during sexual activity, using lubricants and practicing gentle, slow movements can make the experience more comfortable. It is also important to communicate openly with sexual partners about any pain or discomfort to ensure mutual understanding and support. Incorporating self-care routines such as taking warm baths, practicing relaxation techniques before bed, and ensuring adequate sleep can significantly improve overall well-being and reduce perineum pain. Keeping a pain journal to track symptoms and triggers can help identify patterns and make informed decisions about lifestyle adjustments. Consulting healthcare providers for personalized advice on lifestyle changes and self-care strategies tailored to individual needs is also crucial for effective management of perineum pain. By integrating these lifestyle changes and self-care strategies into daily life, women can better manage their symptoms and improve their quality of life.