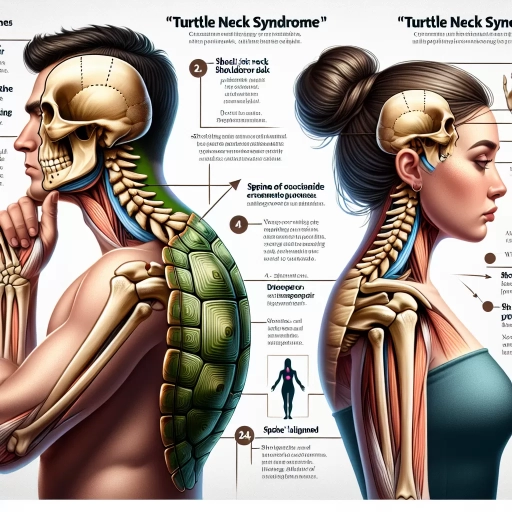
What Is Turtle Neck Syndrome
Turtle neck syndrome, a condition characterized by a forward head posture and an exaggerated curvature of the neck, has become increasingly prevalent in modern society. This syndrome is not merely a cosmetic issue but can lead to significant discomfort, pain, and long-term health complications. Understanding the intricacies of turtle neck syndrome is crucial for both prevention and treatment. This article delves into the definition and overview of turtle neck syndrome, exploring its causes and risk factors, as well as the diagnostic, treatment, and management strategies available. By examining these aspects, individuals can gain a comprehensive understanding of how to identify, address, and mitigate the effects of this condition. To begin, it is essential to grasp the fundamental concept of turtle neck syndrome, which will be detailed in the following section: **Understanding Turtle Neck Syndrome: Definition and Overview**.
Understanding Turtle Neck Syndrome: Definition and Overview
Understanding Turtle Neck Syndrome is a complex and multifaceted topic that requires a comprehensive approach to fully grasp its implications. This condition, characterized by a distinctive posture and set of symptoms, has been studied and documented over various periods, making historical context crucial for its understanding. The historical context provides insights into how the syndrome was first identified and how our understanding of it has evolved over time. Additionally, delving into the medical terminology associated with Turtle Neck Syndrome is essential for a clear and accurate diagnosis. This involves understanding the specific anatomical and physiological changes that occur in individuals affected by this condition. Furthermore, recognizing the common symptoms and clinical presentation is vital for early detection and treatment. Distinguishing Turtle Neck Syndrome from other conditions that may present similar symptoms is also critical to ensure accurate diagnosis and appropriate care. By exploring these aspects, we can gain a deeper understanding of Turtle Neck Syndrome and its impact on those affected. Let us begin by examining the historical context and medical terminology surrounding this condition.
Historical Context and Medical Terminology
To fully grasp the concept of Turtle Neck Syndrome, it is essential to delve into its historical context and the evolution of medical terminology surrounding this condition. Historically, the term "Turtle Neck Syndrome" emerged in the mid-20th century as a colloquialism to describe a specific type of cervical spine injury. This syndrome was first identified in the context of whiplash injuries, particularly those sustained in motor vehicle accidents. The name "Turtle Neck" was coined due to the characteristic posture patients adopted to alleviate pain, resembling the protective stance of a turtle. The medical terminology associated with Turtle Neck Syndrome has evolved significantly over the years. Initially, it was described under broader categories such as cervical sprain or strain. However, as diagnostic techniques improved, particularly with the advent of advanced imaging technologies like MRI and CT scans, healthcare professionals began to recognize distinct patterns of injury that warranted a more specific classification. Today, Turtle Neck Syndrome is often discussed within the framework of cervical facet joint syndrome or cervical facet capsule injury. Understanding the historical development of this condition helps in appreciating the current diagnostic and therapeutic approaches. Early descriptions were largely based on clinical presentations and physical examinations, whereas modern definitions incorporate detailed radiological findings. For instance, the presence of facet joint effusion, capsular tears, and ligamentous injuries are now key components in diagnosing Turtle Neck Syndrome. Moreover, advancements in medical terminology have facilitated better communication among healthcare providers. Terms such as "facet joint arthropathy" and "cervical spine instability" are now commonly used to describe the underlying pathophysiology of Turtle Neck Syndrome. This precision in terminology has led to more targeted treatment strategies, including physical therapy, interventional pain management, and in some cases, surgical intervention. In summary, the historical context and evolution of medical terminology surrounding Turtle Neck Syndrome highlight the importance of continuous medical research and diagnostic advancements. By understanding how this condition has been described and treated over time, healthcare providers can offer more accurate diagnoses and effective treatments, ultimately improving patient outcomes. This historical perspective also underscores the dynamic nature of medical knowledge, emphasizing the need for ongoing education and adaptation in clinical practice.
Common Symptoms and Clinical Presentation
Turtle neck syndrome, a condition characterized by the forward flexion of the neck and an inability to extend it fully, presents with a distinct set of symptoms that can significantly impact an individual's quality of life. Clinically, patients often report severe neck pain and stiffness, which can radiate to the shoulders and upper back. This discomfort is typically exacerbated by movement and may be accompanied by muscle spasms in the cervical region. Another hallmark symptom is limited range of motion in the neck, making everyday activities such as driving, reading, or even simple tasks like looking up or down challenging. Headaches are also a common complaint, often described as dull and aching, and can be attributed to the strain on the muscles and ligaments supporting the head and neck. Some individuals may experience numbness or tingling sensations in the arms or hands due to compression of the cervical nerves. In more severe cases, patients might report dizziness or lightheadedness when changing positions, indicative of potential vertebral artery insufficiency. The clinical presentation of turtle neck syndrome can vary depending on the underlying cause. For instance, if it is due to a degenerative condition like cervical spondylosis, patients may exhibit signs of spinal cord compression such as weakness in the limbs, loss of reflexes, or even bladder and bowel dysfunction. In cases where the syndrome is secondary to an inflammatory process like rheumatoid arthritis, systemic symptoms such as fever, fatigue, and joint pain in other parts of the body may also be present. A thorough physical examination is crucial for diagnosing turtle neck syndrome. Healthcare providers typically assess the patient's posture, range of motion, and muscle strength. Palpation of the neck may reveal tender points and muscle tightness. Neurological examination may include testing reflexes, sensation, and motor function to rule out any neurological deficits. Imaging studies such as X-rays, CT scans, or MRI are often necessary to identify the underlying cause of the syndrome. These diagnostic tools can help visualize any structural abnormalities in the cervical spine, such as herniated discs, bone spurs, or fractures. In some cases, electromyography (EMG) and nerve conduction studies (NCS) may be ordered to evaluate nerve function and rule out other conditions that could mimic turtle neck syndrome. Understanding the clinical presentation and common symptoms of turtle neck syndrome is essential for timely diagnosis and appropriate management. Early recognition allows healthcare providers to implement effective treatment strategies, which may include physical therapy, pain management with medications, or in some cases, surgical intervention to alleviate symptoms and improve the patient's functional status. By addressing these symptoms comprehensively, individuals can regain their mobility and reduce their discomfort, significantly enhancing their overall well-being.
Distinguishing Features from Other Conditions
**Distinguishing Features from Other Conditions** Turtle neck syndrome, characterized by a forward head posture and an exaggerated cervical lordosis, must be carefully differentiated from other conditions that present with similar symptoms. One of the key distinguishing features is the absence of pain or neurological deficits, which are common in conditions like cervical spondylosis or herniated discs. Unlike these conditions, turtle neck syndrome typically does not involve radicular symptoms such as numbness, tingling, or weakness in the extremities. Instead, it is often associated with chronic muscle strain and fatigue due to the prolonged abnormal posture. Another condition that may be confused with turtle neck syndrome is kyphosis, particularly in its cervical form. However, kyphosis involves an abnormal curvature of the spine in the sagittal plane, leading to a rounded appearance of the back, whereas turtle neck syndrome involves an anterior displacement of the head relative to the shoulders. Additionally, kyphosis can be associated with vertebral fractures or degenerative changes, which are not characteristic of turtle neck syndrome. Postural kyphoscoliosis, which combines elements of both kyphosis and scoliosis, also presents differently. This condition involves both lateral and sagittal plane deformities, often resulting in a more complex spinal alignment issue compared to the straightforward forward head posture seen in turtle neck syndrome. Furthermore, conditions like ankylosing spondylitis or rheumatoid arthritis can cause cervical spine deformities but are typically accompanied by systemic symptoms such as joint pain, inflammation, and other systemic manifestations. In contrast, turtle neck syndrome is primarily a postural issue without underlying inflammatory or degenerative disease processes. In clinical practice, a thorough history and physical examination are crucial for distinguishing turtle neck syndrome from these other conditions. Radiographic imaging may also be necessary to rule out structural abnormalities that could mimic the symptoms of turtle neck syndrome. Understanding these distinguishing features is essential for accurate diagnosis and appropriate management strategies tailored to address the specific needs of patients with this condition. By recognizing these differences, healthcare providers can offer targeted interventions such as physical therapy, ergonomic adjustments, and lifestyle modifications to help patients correct their posture and alleviate associated discomfort.
Causes and Risk Factors of Turtle Neck Syndrome
Turtle Neck Syndrome, a condition characterized by the forward flexion of the neck and an inability to extend it fully, is a complex disorder influenced by multiple factors. Understanding the causes and risk factors of this syndrome is crucial for effective diagnosis and treatment. This article delves into three primary areas that contribute to the development of Turtle Neck Syndrome: Genetic Predisposition and Familial Ties, Environmental and Lifestyle Factors, and Underlying Medical Conditions and Comorbidities. Each of these aspects plays a significant role in determining an individual's susceptibility to this condition. Genetic predisposition can set the stage for a higher risk, while environmental and lifestyle factors such as poor posture or repetitive strain can exacerbate the condition. Additionally, underlying medical conditions and comorbidities can further complicate the situation. By examining these interrelated factors, healthcare professionals can develop comprehensive treatment plans tailored to individual needs. Let's begin by exploring how genetic predisposition and familial ties can lay the groundwork for Turtle Neck Syndrome.
Genetic Predisposition and Familial Ties
Genetic predisposition and familial ties play a significant role in the development of various health conditions, including Turtle Neck Syndrome. This syndrome, characterized by a forward head posture and cervical spine misalignment, can be influenced by genetic factors that affect the structure and function of the musculoskeletal system. Individuals with a family history of musculoskeletal disorders, such as scoliosis or other spinal deformities, may have a higher risk of developing Turtle Neck Syndrome due to inherited traits that impact bone density, muscle tone, and joint alignment. For instance, genetic mutations affecting collagen production or bone mineralization can lead to weaker spinal structures, making it more likely for individuals to develop the characteristic forward head posture associated with Turtle Neck Syndrome. Furthermore, familial tendencies towards poor posture or lifestyle habits that contribute to spinal misalignment can also be passed down through generations, exacerbating the risk. Understanding these genetic and familial factors is crucial for early diagnosis and intervention, allowing healthcare providers to implement preventive measures and personalized treatment plans tailored to an individual's specific risk profile. By acknowledging the interplay between genetics and family history, healthcare professionals can better address the underlying causes of Turtle Neck Syndrome, ultimately improving patient outcomes and quality of life. This holistic approach underscores the importance of considering both genetic predisposition and familial ties when assessing the causes and risk factors associated with this condition.
Environmental and Lifestyle Factors
Environmental and lifestyle factors play a significant role in the development and exacerbation of Turtle Neck Syndrome, a condition characterized by forward head posture and associated musculoskeletal issues. One of the primary environmental factors is prolonged exposure to screens, such as computers, smartphones, and televisions. This constant forward leaning to view screens can lead to chronic strain on the neck muscles, contributing to the forward head posture typical of Turtle Neck Syndrome. Additionally, poor ergonomic setups in workplaces and homes, including inadequate chair height, monitor placement, and keyboard positioning, further exacerbate this issue by promoting unhealthy postures. Lifestyle choices also significantly impact the risk of developing Turtle Neck Syndrome. Sedentary lifestyles, which are increasingly common due to modern work habits and leisure activities, contribute to muscle weakness and poor posture. Lack of regular exercise, particularly exercises that strengthen the neck and shoulder muscles, can make individuals more susceptible to this condition. Furthermore, inadequate sleep quality and duration can affect muscle recovery and overall posture, as poor sleep often leads to increased muscle tension and fatigue. Another critical lifestyle factor is stress management. Chronic stress can lead to muscle tightness and poor posture as individuals often unconsciously adopt protective postures when feeling anxious or stressed. This habitual tightening of muscles can contribute to the development of Turtle Neck Syndrome over time. Moreover, dietary habits that lead to obesity or malnutrition can affect overall muscle health and bone density, making it harder for the body to maintain proper posture. In terms of specific activities, certain sports and hobbies that involve repetitive movements or awkward postures can also contribute to Turtle Neck Syndrome. For example, cyclists who spend long hours leaning forward over handlebars or musicians who play instruments requiring forward head positioning are at higher risk. Similarly, individuals who engage in activities that involve heavy lifting or bending without proper technique are more likely to develop musculoskeletal issues that can lead to Turtle Neck Syndrome. Understanding these environmental and lifestyle factors is crucial for both prevention and treatment of Turtle Neck Syndrome. By making conscious choices to improve ergonomics, engage in regular exercise tailored to strengthen neck and shoulder muscles, manage stress effectively, maintain a balanced diet, and adopt healthy sleep habits, individuals can significantly reduce their risk of developing this condition. Additionally, being mindful of posture during daily activities and taking regular breaks to stretch can help mitigate the negative impacts of prolonged screen time and other risk factors associated with modern lifestyles. Addressing these factors not only helps in managing Turtle Neck Syndrome but also contributes to overall health and well-being by promoting better musculoskeletal health and reducing the risk of related conditions such as chronic pain and fatigue.
Underlying Medical Conditions and Comorbidities
**Underlying Medical Conditions and Comorbidities** Turtle Neck Syndrome, characterized by a forward head posture and cervical spine misalignment, is often intertwined with various underlying medical conditions and comorbidities. These underlying factors can significantly exacerbate the symptoms and complicate the treatment of Turtle Neck Syndrome. One of the primary comorbidities is **Chronic Pain**, which can stem from conditions such as fibromyalgia, arthritis, or previous injuries. Chronic pain often leads to muscle tension and poor posture, contributing to the development of Turtle Neck Syndrome. **Neurological Disorders**, including Parkinson's disease, multiple sclerosis, and peripheral neuropathy, can also play a role. These conditions can affect muscle coordination and balance, leading to compensatory postures that strain the cervical spine. **Respiratory Conditions** like chronic obstructive pulmonary disease (COPD) and asthma may also be linked to Turtle Neck Syndrome. Patients with these conditions often adopt a forward-leaning posture to improve lung capacity, which over time can lead to cervical misalignment. **Mental Health Issues**, such as anxiety and depression, are another critical consideration. Individuals suffering from these conditions may exhibit poor posture due to decreased physical activity and altered body mechanics. Additionally, **Sleep Disorders** like sleep apnea and insomnia can contribute to Turtle Neck Syndrome by affecting the quality of sleep and leading to chronic fatigue, which in turn can result in poor posture. **Metabolic Disorders**, including diabetes and obesity, are also relevant comorbidities. Obesity places additional strain on the cervical spine, while diabetes can lead to neuropathy and muscle weakness, both of which can contribute to poor posture. **Gastrointestinal Issues**, such as gastroesophageal reflux disease (GERD), may cause patients to adopt a forward head posture to alleviate symptoms, further straining the cervical spine. Understanding these underlying medical conditions and comorbidities is crucial for developing an effective treatment plan for Turtle Neck Syndrome, as addressing these concurrent issues can significantly improve patient outcomes. By recognizing the interplay between these conditions, healthcare providers can offer more comprehensive care that not only alleviates the symptoms of Turtle Neck Syndrome but also improves overall health and well-being.
Diagnosis, Treatment, and Management of Turtle Neck Syndrome
Turtle Neck Syndrome, a condition characterized by the forward flexion of the neck and chin, poses significant challenges for both patients and healthcare providers. Effective management of this syndrome requires a multifaceted approach that encompasses accurate diagnosis, appropriate treatment, and sustainable lifestyle modifications. The diagnostic process is crucial and involves various techniques and tools to identify the underlying causes of the condition. This includes imaging studies such as X-rays and MRI scans, as well as clinical evaluations to assess muscle strength and range of motion. Once a diagnosis is established, therapeutic approaches can be tailored to address the specific needs of the patient. Treatment options may include physical therapy, medication to manage pain and inflammation, and in some cases, surgical intervention. Additionally, lifestyle modifications play a critical role in long-term management, focusing on posture correction, ergonomic adjustments, and regular exercise to maintain neck mobility and strength. By understanding these diagnostic techniques, therapeutic approaches, and lifestyle modifications, individuals can better navigate the complexities of Turtle Neck Syndrome and achieve optimal outcomes. This article will delve into these aspects, beginning with an exploration of the diagnostic techniques and tools essential for accurately identifying and addressing this condition.
Diagnostic Techniques and Tools
**Diagnostic Techniques and Tools** Diagnosing Turtle Neck Syndrome, a condition characterized by the abnormal curvature of the neck due to muscle spasms or other underlying causes, requires a comprehensive approach that leverages various diagnostic techniques and tools. The initial step often involves a thorough clinical examination where healthcare professionals assess the patient's medical history, perform physical examinations, and evaluate symptoms such as neck pain, stiffness, and limited range of motion. Imaging studies are crucial for confirming the diagnosis and identifying any underlying structural issues. **Radiographic Imaging:** - **X-rays:** Provide initial insights into bone alignment and potential fractures or dislocations. - **Computed Tomography (CT) Scans:** Offer detailed cross-sectional images of the neck, helping to identify soft tissue abnormalities, bony structures, and any signs of degenerative changes. - **Magnetic Resonance Imaging (MRI):** Delivers high-resolution images of soft tissues including muscles, tendons, ligaments, and spinal discs, which is essential for diagnosing conditions like herniated discs or spinal stenosis that may contribute to Turtle Neck Syndrome. **Electrodiagnostic Tests:** - **Electromyography (EMG):** Measures the electrical activity of muscles to detect muscle spasms or other neuromuscular disorders. - **Nerve Conduction Studies (NCS):** Assess the speed and strength of electrical signals traveling through nerves, aiding in the diagnosis of nerve compression or neuropathy. **Other Diagnostic Tools:** - **Blood Tests:** May be conducted to rule out inflammatory or infectious causes of neck pain. - **Physical Therapy Evaluation:** A physical therapist can assess muscle strength, flexibility, and range of motion to identify specific areas of dysfunction. - **Questionnaires and Scales:** Tools like the Neck Disability Index (NDI) help quantify the severity of symptoms and functional impairment. **Advanced Techniques:** - **Dynamic Imaging:** Such as flexion-extension X-rays can reveal instability in the cervical spine. - **Functional MRI:** Provides insights into spinal cord compression during different neck positions. By integrating these diagnostic techniques and tools, healthcare providers can accurately diagnose Turtle Neck Syndrome, identify underlying causes, and develop an effective treatment plan tailored to the individual's needs. This multifaceted approach ensures comprehensive care that addresses both immediate symptoms and long-term management strategies.
Therapeutic Approaches and Treatment Options
Therapeutic approaches and treatment options for Turtle Neck Syndrome, a condition characterized by a forward head posture and associated musculoskeletal discomfort, are multifaceted and tailored to address the underlying causes and symptoms. The primary goal of treatment is to restore proper spinal alignment, alleviate pain, and improve overall posture. **Physical Therapy:** A cornerstone of treatment, physical therapy involves a series of exercises and stretches designed to strengthen the neck and shoulder muscles while improving flexibility. Therapists may use techniques such as manual therapy, including massage and joint mobilization, to reduce muscle tension and enhance range of motion. Postural education is also crucial, teaching patients how to maintain correct posture during daily activities. **Chiropractic Care:** Chiropractors play a significant role in managing Turtle Neck Syndrome by performing spinal manipulations and adjustments to realign the vertebrae and relieve pressure on the muscles and joints. This approach can help restore normal spinal curvature and reduce pain. **Ergonomic Modifications:** Making ergonomic adjustments to the workspace is essential. This includes ensuring that the computer monitor is at eye level, using a supportive chair, and taking regular breaks to stretch. These modifications help reduce strain on the neck and shoulders, preventing exacerbation of the condition. **Pain Management:** For patients experiencing significant pain, various pain management strategies may be employed. Over-the-counter pain relievers such as NSAIDs can provide temporary relief. In more severe cases, prescription medications like muscle relaxants or corticosteroid injections may be necessary. Alternative methods such as acupuncture and heat or cold therapy can also be beneficial. **Orthotics and Assistive Devices:** Custom orthotics, such as cervical collars or posture correctors, can provide additional support and help maintain proper spinal alignment. Assistive devices like ergonomic pillows and back supports can also aid in maintaining good posture during sleep and other activities. **Lifestyle Changes:** Lifestyle modifications are critical for long-term management. Encouraging regular exercise, such as yoga or Pilates, which focus on core strength and flexibility, can help maintain good posture. Reducing screen time and engaging in activities that promote better posture are also recommended. **Surgical Interventions:** In rare cases where conservative treatments fail to provide relief, surgical interventions may be considered. Surgery might involve procedures to correct spinal deformities or relieve compression on nerves. In summary, the therapeutic approaches for Turtle Neck Syndrome are diverse and often involve a combination of physical therapy, chiropractic care, ergonomic adjustments, pain management strategies, orthotics, lifestyle changes, and in some cases, surgical interventions. A comprehensive treatment plan tailored to the individual's needs is key to achieving optimal outcomes and improving quality of life. By addressing both the physical and lifestyle aspects of the condition, patients can experience significant relief from symptoms and improve their overall well-being.
Lifestyle Modifications and Long-Term Management Strategies
**Lifestyle Modifications and Long-Term Management Strategies** Effective management of Turtle Neck Syndrome (TNS) involves a multifaceted approach that includes lifestyle modifications and long-term strategies to alleviate symptoms and prevent exacerbation. At the core of these modifications is maintaining a healthy posture, which can significantly reduce the strain on the neck and shoulder muscles. Regular exercises tailored to strengthen the neck and shoulder muscles, such as simple stretches and isometric exercises, are crucial. For instance, chin tucks and shoulder rolls can help improve muscle tone and flexibility, thereby reducing the likelihood of muscle fatigue and pain. In addition to physical exercises, ergonomic adjustments play a vital role. Ensuring that the workspace is ergonomically set up can help minimize strain on the neck. This includes positioning the computer monitor at eye level, using a supportive chair with proper lumbar support, and taking regular breaks to stand up and stretch. Proper sleeping habits are also essential; using a supportive pillow that maintains the natural curve of the neck can help prevent muscle strain during sleep. Dietary changes can also contribute to long-term management. A balanced diet rich in nutrients such as vitamin D, calcium, and omega-3 fatty acids supports overall muscle health. Staying hydrated is equally important as it helps maintain spinal disc health and overall musculoskeletal well-being. Stress management techniques are another critical component. Stress can exacerbate muscle tension, so practices like meditation, yoga, or deep breathing exercises can help reduce overall stress levels. Furthermore, avoiding heavy lifting or bending activities that strain the neck and shoulders is advisable. For individuals with TNS, regular follow-up appointments with healthcare providers are essential for monitoring progress and adjusting treatment plans as needed. This may include periodic physical therapy sessions to maintain muscle strength and flexibility. In some cases, incorporating alternative therapies such as acupuncture or massage therapy may provide additional relief from symptoms. Adopting a proactive approach to managing TNS involves being mindful of daily activities that could exacerbate the condition. For example, avoiding prolonged periods of sitting or standing in one position and taking regular breaks to move around can help distribute the load more evenly across the muscles. By combining these lifestyle modifications with medical treatment plans, individuals can effectively manage their symptoms over the long term, improving their quality of life significantly. In conclusion, while TNS presents unique challenges, a comprehensive strategy that includes physical exercises, ergonomic adjustments, dietary changes, stress management techniques, and regular healthcare check-ups can significantly mitigate its impact. By integrating these lifestyle modifications into daily routines, individuals can achieve better long-term outcomes and reduce the likelihood of symptom recurrence. This holistic approach not only addresses the immediate symptoms but also fosters a healthier lifestyle that benefits overall well-being.