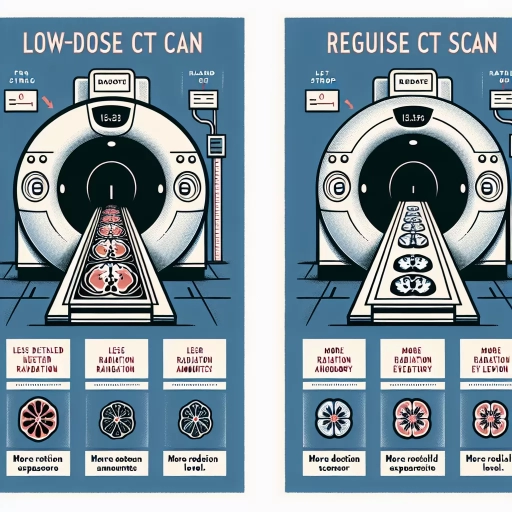
What Is The Difference Between A Low-dose Ct Scan And A Regular Ct Scan
In the realm of medical imaging, Computed Tomography (CT) scans have revolutionized diagnostic capabilities, offering detailed cross-sectional images of the body. However, advancements in technology have led to the development of low-dose CT scans, which differ significantly from their traditional counterparts. Understanding these differences is crucial for both healthcare providers and patients. This article delves into the distinctions between low-dose CT scans and regular CT scans, focusing on three key areas: differences in radiation exposure, technological and methodological differences, and clinical applications and diagnostic accuracy. By exploring these aspects, we can better appreciate how low-dose CT scans are redefining the landscape of medical imaging. Let's begin by examining one of the most critical distinctions: the differences in radiation exposure, which is a paramount concern for patient safety and long-term health outcomes.
Differences in Radiation Exposure
Radiation exposure is a critical concern in medical imaging, particularly with the widespread use of computed tomography (CT) scans. Understanding the differences in radiation exposure is essential for both healthcare providers and patients. This article delves into three key aspects: the lower radiation dose in low-dose CT scans, the impact on patient safety and health risks, and the regulatory guidelines for radiation limits. By examining these facets, we can better appreciate how advancements in technology and stringent regulations are working together to minimize risks associated with radiation exposure. For instance, low-dose CT scans have revolutionized diagnostic imaging by significantly reducing the amount of radiation patients are exposed to, making them a safer alternative for routine check-ups and follow-ups. This reduction in radiation dose is particularly important as it directly impacts patient safety and health risks, such as the potential for cancer and other long-term health issues. Furthermore, regulatory guidelines play a crucial role in ensuring that these lower doses are implemented consistently across medical facilities. Let's start by exploring how lower radiation doses in low-dose CT scans are transforming the landscape of medical imaging.
1. Lower Radiation Dose in Low-Dose CT Scans
One of the most significant differences between a low-dose CT scan and a regular CT scan is the radiation dose exposure. Low-dose CT scans are designed to minimize radiation exposure while still providing high-quality images, making them particularly beneficial for patients who require frequent scans or those with conditions that necessitate long-term monitoring. The technology behind low-dose CT scans involves advanced algorithms and improved detector systems that enhance image quality even at lower radiation levels. This reduction in radiation dose is crucial because it decreases the cumulative risk of radiation-induced health issues, such as cancer and genetic mutations, which are concerns associated with higher doses of ionizing radiation. In practice, low-dose CT scans achieve this reduction through several mechanisms. For instance, they often use lower X-ray tube voltages and currents, which directly reduce the amount of radiation emitted. Additionally, modern CT scanners employ sophisticated software that can reconstruct high-quality images from fewer data points, thereby allowing for lower doses without compromising diagnostic accuracy. These advancements have been particularly significant in areas like lung cancer screening, where low-dose CT scans have become the standard due to their ability to detect early-stage tumors with minimal radiation exposure. Moreover, the development of iterative reconstruction techniques has played a pivotal role in enabling low-dose CT scans. These techniques involve complex algorithms that iteratively refine image data to produce clearer images from lower doses of radiation. This not only reduces patient exposure but also enhances the diagnostic confidence of healthcare providers by providing detailed and accurate images. Furthermore, some newer CT scanners incorporate artificial intelligence (AI) and machine learning (ML) to optimize image quality further, ensuring that even at lower doses, the diagnostic information remains robust. The clinical implications of lower radiation doses in low-dose CT scans are profound. For pediatric patients, who are more sensitive to radiation due to their developing tissues, low-dose protocols are essential for minimizing long-term risks. Similarly, for patients undergoing serial scans for conditions like chronic obstructive pulmonary disease (COPD) or cystic fibrosis, reducing cumulative radiation exposure is critical for their overall health and safety. The widespread adoption of low-dose CT scans reflects a broader shift in medical imaging towards patient-centered care that balances diagnostic needs with safety considerations. In conclusion, the lower radiation dose in low-dose CT scans represents a significant advancement in medical imaging technology. By leveraging cutting-edge software, improved detector systems, and innovative reconstruction techniques, these scans offer a safer alternative to traditional CT scans without compromising on image quality or diagnostic accuracy. As healthcare continues to evolve, the importance of minimizing radiation exposure will only grow, making low-dose CT scans an indispensable tool in modern clinical practice.
2. Impact on Patient Safety and Health Risks
The impact on patient safety and health risks is a critical consideration when comparing low-dose CT scans to regular CT scans. One of the primary differences lies in the amount of radiation exposure, which directly influences the risk of radiation-induced health issues. Regular CT scans, while highly effective for diagnostic purposes, involve higher doses of ionizing radiation. This increased exposure can elevate the risk of developing cancer and other health problems over time, particularly in younger patients and those undergoing multiple scans. In contrast, low-dose CT scans are designed to minimize radiation exposure while still providing accurate diagnostic images. By using advanced technologies such as iterative reconstruction algorithms and improved detector materials, low-dose CT scans can reduce radiation doses by up to 50% or more without compromising image quality. This reduction significantly lowers the long-term health risks associated with radiation, making low-dose CT scans a safer option for patients who require frequent or repeated imaging. Moreover, the reduced radiation exposure in low-dose CT scans is particularly beneficial for vulnerable populations such as children and pregnant women. For these groups, even small amounts of radiation can pose significant health risks due to their higher sensitivity and longer life expectancy. By opting for low-dose CT scans, healthcare providers can ensure that these patients receive necessary diagnostic information without exposing them to unnecessary radiation. Additionally, the use of low-dose protocols aligns with the principle of ALARA (As Low As Reasonably Achievable), which is a guiding principle in medical imaging aimed at minimizing patient exposure to ionizing radiation while maintaining diagnostic efficacy. From a patient safety perspective, the adoption of low-dose CT scans also fosters greater confidence and compliance with medical imaging recommendations. Patients who are aware of the reduced health risks associated with low-dose scans may be more likely to adhere to prescribed imaging schedules, leading to better health outcomes. Furthermore, the integration of low-dose protocols into clinical practice encourages a culture of safety within healthcare institutions, promoting continuous improvement in patient care and risk management. In summary, the impact on patient safety and health risks is a compelling reason to prefer low-dose CT scans over regular ones. By significantly reducing radiation exposure, these scans mitigate long-term health risks such as cancer and other radiation-induced conditions. This makes them an essential tool in modern healthcare, especially for sensitive populations and those requiring frequent imaging. As technology continues to evolve, the development and widespread adoption of low-dose CT protocols will play a crucial role in enhancing patient safety and improving overall health outcomes.
3. Regulatory Guidelines for Radiation Limits
Regulatory guidelines for radiation limits play a crucial role in ensuring the safety of patients undergoing medical imaging procedures, including CT scans. These guidelines are established by various international and national bodies to protect individuals from the potential risks associated with ionizing radiation. The International Commission on Radiological Protection (ICRP) and the National Council on Radiation Protection and Measurements (NCRP) are among the key organizations that set standards for radiation exposure limits. For medical imaging, the principle of "as low as reasonably achievable" (ALARA) is paramount. This principle mandates that healthcare providers use the lowest dose of radiation necessary to achieve diagnostic-quality images. Regulatory bodies enforce this through strict guidelines on dose limits and quality control measures. For instance, the U.S. Food and Drug Administration (FDA) has specific regulations regarding the performance standards for CT scanners, including requirements for dose monitoring and reporting. In the context of CT scans, regulatory guidelines differentiate between diagnostic and therapeutic uses of radiation. Diagnostic CT scans, whether low-dose or regular, must adhere to guidelines that ensure patient safety while maintaining image quality. The American College of Radiology (ACR) and the Radiological Society of North America (RSNA) collaborate to develop appropriateness criteria and guidelines for CT scan usage, emphasizing the importance of justifying each scan based on clinical necessity. Low-dose CT scans, in particular, have gained attention due to their ability to reduce radiation exposure without significantly compromising image quality. Regulatory guidelines support the use of low-dose protocols by providing frameworks for optimizing scan parameters such as tube voltage, current, and slice thickness. These adjustments help in minimizing the dose while preserving diagnostic accuracy. Moreover, regulatory bodies advocate for ongoing education and training for healthcare professionals to ensure they are aware of and adhere to current guidelines. This includes regular updates on new technologies and best practices in radiation safety. By enforcing these guidelines, regulatory agencies help mitigate the risks associated with radiation exposure, thereby enhancing patient safety and outcomes. In summary, regulatory guidelines for radiation limits are essential in governing the safe use of CT scans. By adhering to these guidelines, healthcare providers can balance the need for diagnostic accuracy with the necessity of minimizing patient exposure to ionizing radiation. This balanced approach is critical in ensuring that both low-dose and regular CT scans are performed in a manner that prioritizes patient safety while maintaining high standards of medical care.
Technological and Methodological Differences
The field of medical imaging has witnessed significant advancements in recent years, driven by technological and methodological innovations. These developments have not only enhanced the accuracy and detail of diagnostic images but also expanded the range of applications for imaging technologies. Three key areas highlight these advancements: advanced imaging algorithms and software, variations in scanner settings and protocols, and the use of contrast agents and their effects. Advanced imaging algorithms and software have revolutionized image processing, enabling faster and more precise diagnostics. Variations in scanner settings and protocols allow for tailored imaging strategies that optimize data acquisition for different clinical scenarios. Additionally, the strategic use of contrast agents has improved the visibility of specific anatomical structures, aiding in more accurate diagnoses. Understanding these differences is crucial for healthcare professionals to leverage the full potential of modern imaging technologies. This article delves into these critical aspects, starting with the transformative impact of advanced imaging algorithms and software.
1. Advanced Imaging Algorithms and Software
Advanced imaging algorithms and software play a pivotal role in the technological and methodological differences between low-dose CT scans and regular CT scans. These sophisticated tools are designed to enhance image quality while minimizing radiation exposure, making them indispensable for modern diagnostic imaging. At the heart of these advancements are iterative reconstruction algorithms, which significantly improve image resolution and reduce noise compared to traditional filtered back projection methods. For instance, techniques like Adaptive Statistical Iterative Reconstruction (ASIR) and Model-Based Iterative Reconstruction (MBIR) leverage complex mathematical models to reconstruct images from fewer data points, thereby allowing for lower doses of radiation without compromising diagnostic accuracy. Moreover, advanced software solutions integrate machine learning and artificial intelligence to optimize image processing. These AI-driven algorithms can automatically adjust parameters to achieve the best possible image quality based on patient-specific factors, such as body type and the area being scanned. This personalized approach ensures that each scan is tailored to minimize radiation exposure while maintaining the necessary diagnostic detail. Additionally, software enhancements like noise reduction filters and edge enhancement tools further refine the images, making subtle abnormalities more discernible even at lower doses. Another key aspect is the integration of deep learning techniques, which enable the development of more accurate and efficient imaging protocols. Deep learning models can be trained on vast datasets to recognize patterns and anomalies that might be missed by human interpreters, thereby enhancing diagnostic precision. These models also facilitate real-time feedback during the scanning process, allowing technicians to adjust settings on the fly to ensure optimal image quality with minimal radiation. The impact of these advanced imaging algorithms and software extends beyond just reducing radiation doses; they also contribute to faster scan times and improved patient comfort. By streamlining the scanning process and reducing the need for repeat scans, these technologies help in managing healthcare resources more efficiently. Furthermore, they support the development of personalized medicine by enabling more precise and detailed imaging that can be tailored to individual patient needs. In summary, advanced imaging algorithms and software are crucial in bridging the gap between low-dose CT scans and regular CT scans by providing high-quality images with reduced radiation exposure. These technological advancements not only enhance diagnostic capabilities but also contribute to better patient outcomes and more efficient healthcare practices. As these technologies continue to evolve, they promise even greater improvements in the field of diagnostic imaging, making low-dose CT scans an increasingly viable option for a wide range of medical applications.
2. Variations in Scanner Settings and Protocols
Variations in scanner settings and protocols play a crucial role in distinguishing between low-dose CT scans and regular CT scans, highlighting the technological and methodological differences that underpin these imaging techniques. At the heart of these variations lies the adjustment of key parameters such as X-ray tube current, voltage, and exposure time. In low-dose CT scans, these settings are optimized to minimize radiation exposure while maintaining diagnostic image quality. For instance, the X-ray tube current is often reduced, which decreases the dose of radiation delivered to the patient. Additionally, advanced reconstruction algorithms and noise reduction techniques are employed to enhance image clarity despite lower radiation levels. Protocols also differ significantly between low-dose and regular CT scans. Low-dose protocols typically involve thinner slice thicknesses and smaller field-of-view settings to focus on specific areas of interest, thereby reducing overall radiation exposure. In contrast, regular CT scans may use thicker slice thicknesses and larger field-of-views to capture more comprehensive images, albeit at higher doses of radiation. The use of iterative reconstruction techniques in low-dose protocols further aids in reducing noise and improving image resolution without increasing the radiation dose. Moreover, modern CT scanners often come equipped with automated dose modulation systems that dynamically adjust X-ray tube current based on patient size and anatomy, ensuring optimal image quality with minimal radiation. These systems are particularly beneficial in low-dose protocols where maintaining diagnostic accuracy is paramount despite reduced radiation levels. Furthermore, advancements in detector technology have enabled newer scanners to capture high-quality images at lower doses by improving sensitivity and reducing noise. The choice of scanner settings and protocols also depends on the specific clinical application. For example, in pediatric imaging or follow-up scans where cumulative radiation dose is a concern, low-dose protocols are preferred. Conversely, in cases requiring detailed anatomical information such as pre-surgical planning or complex trauma assessments, regular CT scan settings may be necessary to ensure sufficient image detail. In summary, variations in scanner settings and protocols are fundamental to the distinction between low-dose and regular CT scans. By carefully adjusting parameters like X-ray tube current and employing advanced reconstruction techniques, healthcare providers can achieve high-quality diagnostic images while minimizing patient exposure to radiation. These methodological differences underscore the evolving landscape of CT technology aimed at balancing diagnostic efficacy with patient safety.
3. Use of Contrast Agents and Their Effects
The use of contrast agents in CT scans is a critical aspect that highlights significant technological and methodological differences between low-dose CT scans and regular CT scans. Contrast agents, typically iodine-based or barium-based substances, are administered to enhance the visibility of internal structures by altering the X-ray absorption properties of tissues. In regular CT scans, these agents are often used liberally to provide clear delineation between different tissues and organs, which is particularly beneficial for diagnosing conditions such as tumors, vascular diseases, and inflammatory processes. However, the use of contrast agents comes with potential risks, including allergic reactions, kidney damage (nephrotoxicity), and increased radiation exposure due to the need for higher doses to achieve optimal contrast. In contrast, low-dose CT scans aim to minimize radiation exposure while still providing diagnostic-quality images. Here, the use of contrast agents is more judicious and often limited to cases where it is absolutely necessary. Advanced imaging technologies such as iterative reconstruction algorithms and dual-energy CT scanners help improve image quality without relying heavily on contrast agents. These technologies can differentiate between various tissues based on their inherent properties rather than relying on the enhancement provided by contrast media. For instance, dual-energy CT can distinguish between iodine and calcium, allowing for better characterization of lesions without the need for high doses of contrast. Moreover, low-dose CT protocols often incorporate patient-specific factors such as body size and the specific clinical question being addressed to determine whether contrast is truly necessary. This tailored approach not only reduces the risk associated with contrast agents but also aligns with the principle of ALARA (As Low As Reasonably Achievable) in radiation exposure. Additionally, advancements in software and hardware have enabled the development of low-contrast or no-contrast protocols that leverage sophisticated image processing techniques to enhance image quality without the administration of exogenous substances. The effects of these differences are multifaceted. For patients, reduced use of contrast agents in low-dose CT scans translates into lower risks of adverse reactions and long-term health consequences. Clinically, it means that diagnostic accuracy can be maintained or even improved through innovative imaging techniques rather than relying solely on contrast enhancement. From a healthcare perspective, this shift towards more judicious use of contrast agents can lead to cost savings and improved patient safety profiles. Overall, the strategic use of contrast agents in low-dose CT scans underscores a broader trend towards personalized medicine and responsible use of medical technology, highlighting how technological advancements can drive methodological changes that benefit both patients and healthcare systems.
Clinical Applications and Diagnostic Accuracy
The clinical applications and diagnostic accuracy of imaging technologies, particularly CT scans, have revolutionized healthcare by providing precise and timely diagnoses. This article delves into the multifaceted benefits of these technologies, focusing on three key areas: specific indications for low-dose CT scans, comparative diagnostic accuracy and sensitivity, and patient populations benefiting from each type of imaging. Understanding the specific indications for low-dose CT scans is crucial as it allows healthcare providers to balance the need for detailed imaging with the risk of radiation exposure. Additionally, comparing the diagnostic accuracy and sensitivity of different imaging modalities helps in selecting the most appropriate tool for various clinical scenarios. Finally, identifying the patient populations that benefit most from each type of imaging ensures that care is tailored to individual needs. By exploring these aspects, healthcare professionals can make informed decisions that enhance patient outcomes. Let us begin by examining the specific indications for low-dose CT scans, a critical component in modern diagnostic practices.
1. Specific Indications for Low-Dose CT Scans
**Specific Indications for Low-Dose CT Scans** Low-dose CT scans are increasingly recognized for their clinical utility in various diagnostic scenarios, particularly where the balance between diagnostic accuracy and radiation exposure is critical. One of the most prominent indications for low-dose CT scans is in lung cancer screening. The National Lung Screening Trial (NLST) demonstrated that annual low-dose CT scans can significantly reduce mortality from lung cancer among high-risk populations, such as heavy smokers. This protocol leverages the sensitivity of CT technology to detect small lung nodules at an early stage when they are more treatable, all while minimizing the cumulative radiation dose over multiple years of screening. Another key indication is in pediatric imaging. Children are more susceptible to the long-term effects of radiation due to their smaller size and longer life expectancy. Low-dose CT protocols are tailored to minimize exposure while still providing high-quality images necessary for diagnosing conditions such as appendicitis, pneumonia, and congenital anomalies. These protocols often involve adjusting the X-ray tube voltage and current, using iterative reconstruction algorithms, and employing pediatric-specific scanning parameters to optimize image quality at lower doses. In addition, low-dose CT scans are beneficial in follow-up imaging for patients with known conditions. For instance, patients undergoing surveillance for previously treated cancers or those with chronic conditions like cystic fibrosis may require frequent CT scans. By using low-dose protocols, healthcare providers can monitor disease progression or response to treatment without subjecting patients to excessive radiation over time. Furthermore, low-dose CT scans are advantageous in emergency settings where rapid diagnosis is crucial but radiation exposure needs to be minimized. In cases of acute abdominal pain or trauma, low-dose CT can quickly provide diagnostic information necessary for immediate treatment decisions while reducing the risk associated with higher doses of radiation. The use of low-dose CT scans also extends to musculoskeletal imaging, particularly for conditions like osteoporosis and fractures. Here, the goal is to assess bone density and integrity with minimal radiation exposure, which is especially important for patients who may require repeated scans over their lifetime. In summary, low-dose CT scans offer a valuable diagnostic tool across a range of clinical applications by balancing the need for accurate imaging with the imperative to minimize radiation exposure. By carefully selecting and optimizing scanning parameters based on patient-specific needs and clinical contexts, healthcare providers can enhance patient safety while maintaining diagnostic accuracy. This approach underscores the evolving role of low-dose CT technology in modern medical practice, aligning with broader efforts to ensure responsible use of ionizing radiation in healthcare.
2. Comparative Diagnostic Accuracy and Sensitivity
When comparing the diagnostic accuracy and sensitivity of low-dose CT scans to regular CT scans, several key factors come into play. Diagnostic accuracy refers to the ability of a test to correctly identify those with and without a particular condition, while sensitivity specifically measures the test's ability to detect true positives. In the context of CT scans, these metrics are crucial for ensuring that patients receive accurate diagnoses without unnecessary exposure to radiation. Low-dose CT scans, as the name suggests, use significantly lower doses of radiation compared to traditional or regular CT scans. This reduction in radiation is particularly beneficial for patients who require frequent imaging, such as those undergoing long-term monitoring for conditions like lung cancer or chronic obstructive pulmonary disease (COPD). Despite the lower radiation dose, advancements in technology have allowed low-dose CT scans to maintain high diagnostic accuracy. For instance, improvements in detector sensitivity and image reconstruction algorithms enable these scans to produce high-quality images that are comparable to those obtained from regular CT scans. Studies have shown that low-dose CT scans can achieve similar diagnostic accuracy for various conditions, including lung nodules and vascular diseases, when compared to standard-dose CT scans. For example, in lung cancer screening, low-dose CT has been demonstrated to have a high sensitivity for detecting small lung nodules, which are often indicative of early-stage cancer. This is particularly important because early detection significantly improves survival rates. However, there are scenarios where regular CT scans may still offer superior diagnostic sensitivity. In cases requiring detailed imaging of complex anatomical structures or in patients with larger body sizes, higher doses of radiation may be necessary to achieve optimal image quality. Additionally, certain conditions such as acute trauma or complex vascular diseases might necessitate the use of standard-dose CT scans to ensure that all relevant details are captured accurately. In summary, while low-dose CT scans offer a compelling balance between reduced radiation exposure and maintained diagnostic accuracy, the choice between low-dose and regular CT scans should be tailored to the specific clinical context. Clinicians must weigh the benefits of reduced radiation against the need for detailed imaging, ensuring that patients receive the most appropriate and effective diagnostic approach for their condition. This nuanced approach underscores the importance of ongoing research and technological advancements aimed at enhancing both the safety and efficacy of CT scanning technologies. By doing so, healthcare providers can optimize patient care while minimizing potential risks associated with radiation exposure.
3. Patient Populations Benefiting from Each Type
When comparing low-dose CT scans to regular CT scans, it is crucial to consider the patient populations that benefit most from each type. **Pediatric patients** significantly benefit from low-dose CT scans due to their higher sensitivity to radiation and the potential long-term risks associated with cumulative radiation exposure. Low-dose protocols are designed to minimize radiation while still providing diagnostic-quality images, making them particularly advantageous for children who may require multiple scans over their lifetime. This approach helps in reducing the risk of radiation-induced cancers and other adverse effects. **Pregnant women** also stand to gain from low-dose CT scans when imaging is absolutely necessary. Although ultrasound and MRI are generally preferred during pregnancy, there are instances where a CT scan is unavoidable. In such cases, using low-dose protocols can help in minimizing fetal exposure to radiation, thereby reducing potential risks to the developing fetus. This cautious approach ensures that diagnostic needs are met without compromising maternal or fetal safety. **Obese patients**, on the other hand, often require regular or even higher-dose CT scans due to their body composition. The increased tissue density in obese individuals can necessitate higher doses of radiation to achieve adequate image quality. However, advancements in technology have led to the development of specialized algorithms and hardware that can optimize image quality even at lower doses for obese patients. Despite this, regular or higher-dose scans may still be necessary in some cases to ensure accurate diagnoses. In contrast, **adults undergoing routine screenings** or those requiring frequent follow-ups for conditions like lung nodules or liver lesions may benefit from regular CT scans if they do not fall into high-risk categories for radiation exposure. Regular CT scans provide high-resolution images that are critical for precise diagnoses and monitoring disease progression. For these patients, the diagnostic accuracy offered by standard doses outweighs the risks associated with radiation. In summary, patient populations such as pediatric patients and pregnant women derive substantial benefits from low-dose CT scans due to their vulnerability to radiation effects. Conversely, obese patients and adults requiring precise diagnostic imaging may necessitate regular or higher-dose scans to ensure optimal image quality and diagnostic accuracy. Understanding these differences is essential for clinicians to make informed decisions that balance diagnostic needs with patient safety.